Posaconazole stands as a formidable antifungal agent, playing a critical role in combating a range of fungal infections. This medication, often prescribed for serious infections, targets a specific group of fungi, effectively disrupting their growth and preventing further spread. Posaconazole’s unique mechanism of action makes it a valuable tool in the fight against fungal diseases, particularly in situations where other antifungal treatments have proven ineffective.
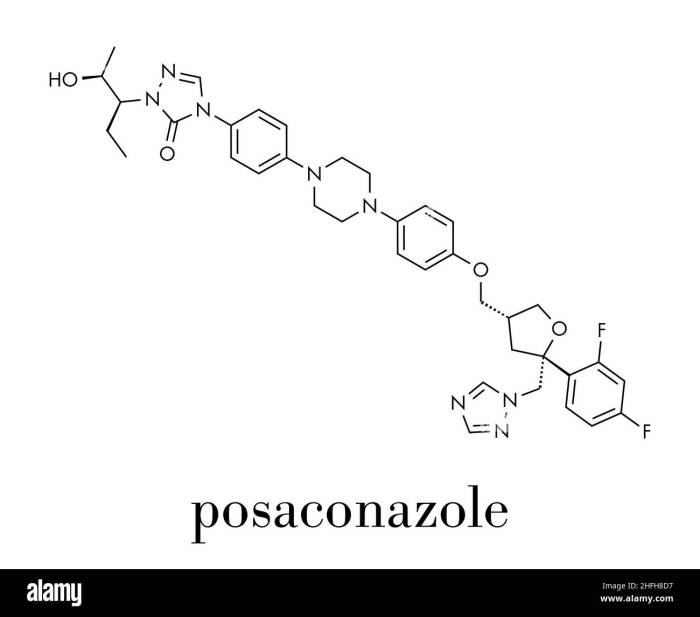
The journey of posaconazole begins with its chemical structure, a complex arrangement of atoms designed to interact with fungal cells. Its impact on these cells, hindering their ability to build essential components, ultimately leads to the demise of the fungal infection. This intricate process, carefully orchestrated by posaconazole, underscores the power of this medication in treating a variety of fungal infections.
Posaconazole
Posaconazole is a broad-spectrum antifungal medication that is used to treat a variety of fungal infections, particularly those caused by Aspergillus and Candida species. It is available in both oral and intravenous formulations and is typically administered for 14 days.
Chemical Structure and Properties
Posaconazole is a triazole antifungal agent with a complex chemical structure. Its molecular formula is C24H22F3N5O4, and its molecular weight is 513.47 g/mol. It is a white to off-white crystalline powder that is practically insoluble in water but soluble in organic solvents such as methanol and ethanol.
Mechanisms of Action
Posaconazole is a potent inhibitor of fungal cytochrome P450 (CYP) enzymes, particularly CYP3A4, which is essential for the biosynthesis of ergosterol, a key component of fungal cell membranes. By inhibiting CYP3A4, posaconazole disrupts the synthesis of ergosterol, leading to cell membrane dysfunction and ultimately fungal cell death.
Therapeutic Uses of Posaconazole
Posaconazole is a broad-spectrum antifungal medication used to treat a variety of fungal infections. It is available in both oral and intravenous formulations, making it suitable for treating various types of fungal infections, including those that are difficult to treat with other antifungal medications.
Specific Indications for Posaconazole
Posaconazole is indicated for the treatment of various fungal infections in specific clinical settings. These include:
- Invasive aspergillosis (IA): Posaconazole is effective in treating IA, particularly in patients who are immunocompromised, such as those with neutropenia or those undergoing hematopoietic stem cell transplantation. It is also used as prophylaxis against IA in high-risk patients.
- Invasive candidiasis (IC): Posaconazole is an effective treatment option for IC, including candidemia, esophageal candidiasis, and disseminated candidiasis. It is particularly useful in patients who are refractory or intolerant to other antifungal medications.
- Mucormycosis: Posaconazole has been shown to be effective in treating mucormycosis, a rare but serious fungal infection that can affect the sinuses, lungs, brain, and other organs. It is often used in combination with other antifungal medications.
- Fungal infections in patients with hematologic malignancies: Posaconazole is frequently used to treat fungal infections in patients with hematologic malignancies, such as leukemia and lymphoma, who are at high risk for developing fungal infections due to their weakened immune systems.
- Prophylaxis of fungal infections in high-risk patients: Posaconazole is used as prophylaxis to prevent fungal infections in patients who are at high risk, such as those undergoing solid organ transplantation, those with prolonged neutropenia, or those receiving chemotherapy.
Efficacy of Posaconazole Compared to Other Antifungal Medications
Posaconazole has been shown to be effective in treating various fungal infections. In clinical trials, posaconazole has demonstrated comparable efficacy to other antifungal medications, such as voriconazole and itraconazole, for treating IA and IC. However, posaconazole may be more effective in treating certain types of fungal infections, such as mucormycosis, compared to other antifungal medications.
Posaconazole has a favorable safety profile and is generally well-tolerated. The most common side effects are gastrointestinal disturbances, such as nausea, vomiting, and diarrhea.
Pharmacokinetics and Metabolism: Posaconazole
Posaconazole’s pharmacokinetic profile is complex, influenced by factors such as formulation, route of administration, and individual patient characteristics. Understanding these aspects is crucial for optimizing posaconazole therapy and achieving desired therapeutic outcomes.
Absorption
Posaconazole’s absorption is influenced by the formulation and route of administration. Oral absorption is generally low, but it can be enhanced by taking posaconazole with a high-fat meal. The bioavailability of posaconazole is approximately 4% for the oral suspension and 15% for the delayed-release tablets.
Distribution
Posaconazole is highly lipophilic and extensively distributed throughout the body, with high concentrations found in the liver, lungs, skin, and cerebrospinal fluid. Posaconazole binds extensively to plasma proteins, with a protein binding rate of approximately 98%.
Metabolism
Posaconazole is primarily metabolized by the cytochrome P450 (CYP) enzyme system, specifically by CYP3A4.
CYP3A4 is a major enzyme involved in the metabolism of many drugs, and its activity can be influenced by various factors, including other medications, food, and genetics.
Posaconazole is a potent inhibitor of CYP3A4, meaning it can slow down the metabolism of other drugs that are also substrates of this enzyme. This can lead to increased levels of these drugs in the body, potentially increasing the risk of side effects.
Excretion
Posaconazole is primarily excreted in the feces, with only a small amount excreted in the urine.
Factors Influencing Posaconazole Pharmacokinetics
Several factors can influence posaconazole pharmacokinetics, including:
- Formulation: The formulation of posaconazole can significantly affect its absorption. The delayed-release tablets have higher bioavailability compared to the oral suspension.
- Route of administration: Oral administration is the most common route, but posaconazole can also be administered intravenously.
- Food: Posaconazole absorption is enhanced when taken with a high-fat meal.
- Concomitant medications: Drugs that inhibit or induce CYP3A4 activity can affect posaconazole metabolism and plasma levels.
- Patient factors: Factors such as age, gender, liver function, and kidney function can also influence posaconazole pharmacokinetics.
Role of Cytochrome P450 Enzymes in Posaconazole Metabolism
Posaconazole is a potent inhibitor of CYP3A4, which is the primary enzyme responsible for its metabolism. This means that posaconazole can increase the levels of other drugs that are also metabolized by CYP3A4.
Posaconazole can interact with other drugs that are metabolized by CYP3A4, potentially leading to increased levels of these drugs in the body and an increased risk of side effects.
Dosage and Administration
Posaconazole is available in various dosage forms, and its administration depends on the type of infection and patient factors. This section delves into the different dosage forms, recommended regimens, administration routes, and considerations for posaconazole.
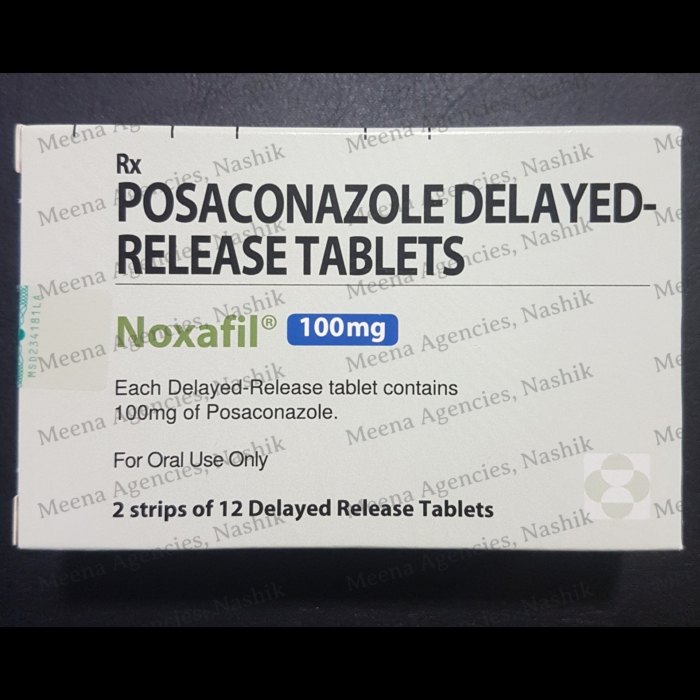
Dosage Forms
Posaconazole is available in three primary dosage forms:
- Oral Suspension: This form is commonly used for patients who can swallow the medication. The suspension is typically administered twice daily, with each dose containing 100 mg of posaconazole.
- Oral Tablets: These tablets are designed for patients who can swallow solid medications. Each tablet contains 100 mg of posaconazole and is usually taken once daily.
- Intravenous (IV) Formulation: The IV formulation is reserved for patients who cannot take oral medications. It is administered as a slow infusion over 1 hour, typically once daily. The IV formulation contains 375 mg of posaconazole in a single vial.
Recommended Dosage Regimens
The recommended dosage regimen for posaconazole varies depending on the type of infection and the patient’s clinical status.
- Invasive Aspergillosis: For patients with invasive aspergillosis, the recommended oral dose is 200 mg twice daily for the first 2 days, followed by 100 mg twice daily. The IV formulation is given at a dose of 375 mg once daily.
- Candidemia and Other Invasive Candidiasis: For patients with candidemia or other invasive candidiasis, the recommended oral dose is 200 mg twice daily for the first 2 days, followed by 100 mg twice daily. The IV formulation is given at a dose of 375 mg once daily.
- Prophylaxis of Invasive Fungal Infections: For prophylaxis of invasive fungal infections in patients at high risk, the recommended oral dose is 100 mg once daily. The IV formulation is given at a dose of 375 mg once daily.
Administration Routes
Posaconazole can be administered orally or intravenously.
- Oral Administration: Oral posaconazole should be taken with a high-fat meal, as this improves its absorption. It is important to swallow the capsules whole and not crush or chew them.
- Intravenous Administration: The IV formulation of posaconazole is administered as a slow infusion over 1 hour. It should be diluted in a compatible IV solution before administration.
Considerations for Posaconazole Administration
Several factors should be considered when administering posaconazole:
- Hepatic Impairment: Patients with severe hepatic impairment may require dose adjustments.
- Drug Interactions: Posaconazole can interact with several other medications, including certain antiretrovirals, statins, and immunosuppressants. It is important to discuss all medications with a healthcare professional before starting posaconazole.
- Monitoring: Regular monitoring of liver function and blood counts is recommended during posaconazole therapy.
Adverse Effects and Drug Interactions
Posaconazole, like many other medications, can cause adverse effects and interact with other drugs. Understanding these potential issues is crucial for safe and effective treatment.
Common Adverse Effects
Common adverse effects of posaconazole are generally mild and manageable.
- Gastrointestinal Issues: Nausea, vomiting, diarrhea, and abdominal pain are the most frequently reported adverse effects. These issues are usually mild and can often be managed with supportive measures, such as taking posaconazole with food or adjusting the dosage.
- Hepatic Effects: Posaconazole can increase liver enzyme levels, potentially leading to liver damage. Regular monitoring of liver function is essential, especially in patients with pre-existing liver disease. Early detection and management of liver dysfunction are crucial.
- Skin Reactions: Rash, itching, and other skin reactions can occur. Most are mild and resolve on their own, but severe reactions may require discontinuation of posaconazole.
- Prolonged QT Interval: Posaconazole can prolong the QT interval on an electrocardiogram (ECG), which can increase the risk of potentially life-threatening arrhythmias. This risk is higher in patients with pre-existing heart conditions. Close monitoring of ECGs is recommended, particularly in high-risk individuals.
Serious Adverse Effects
While less common, posaconazole can also cause serious adverse effects.
- Hepatotoxicity: In rare cases, posaconazole can cause severe liver damage, including liver failure. This risk is increased in patients with pre-existing liver disease or who are taking other medications that can affect the liver. Close monitoring of liver function is crucial. Early signs of liver dysfunction should be promptly investigated and managed.
- Cardiac Arrhythmias: Prolonged QT interval can lead to life-threatening cardiac arrhythmias, such as torsades de pointes. This risk is higher in patients with pre-existing heart conditions, electrolyte imbalances, or who are taking other medications that can prolong the QT interval. Careful monitoring of ECGs and electrolyte levels is crucial.
- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN): Posaconazole can cause these rare but potentially fatal skin reactions. Early recognition and prompt management are crucial to minimize the risk of complications.
Drug Interactions
Posaconazole can interact with a wide range of medications, potentially affecting their effectiveness or increasing the risk of adverse effects.
- CYP3A4 Inhibitors: Posaconazole is a potent inhibitor of CYP3A4, an enzyme involved in the metabolism of many medications. Co-administration with other CYP3A4 inhibitors can lead to increased levels of these medications, potentially causing toxicity. Examples of CYP3A4 inhibitors include clarithromycin, erythromycin, itraconazole, ketoconazole, and grapefruit juice.
- CYP3A4 Substrates: Posaconazole can increase the levels of medications that are metabolized by CYP3A4, leading to increased therapeutic effects or adverse effects. Examples of CYP3A4 substrates include statins, calcium channel blockers, and anti-rejection medications.
- P-glycoprotein Substrates: Posaconazole is also a substrate and inhibitor of P-glycoprotein, a transporter protein involved in drug absorption and elimination. Co-administration with other P-glycoprotein substrates or inhibitors can affect the absorption and elimination of both posaconazole and the other medication.
- Oral Contraceptives: Posaconazole can decrease the effectiveness of oral contraceptives. Alternative contraceptive methods should be considered during posaconazole therapy.
Managing Adverse Effects and Drug Interactions
- Close Monitoring: Regular monitoring of liver function, ECGs, and electrolyte levels is essential to detect and manage potential adverse effects.
- Dosage Adjustment: In some cases, adjusting the dosage of posaconazole or the interacting medication may be necessary to minimize the risk of adverse effects.
- Alternative Medications: If significant adverse effects or drug interactions occur, alternative antifungal medications may be considered.
- Patient Education: Patients should be educated about the potential adverse effects and drug interactions of posaconazole and advised to report any unusual symptoms to their healthcare provider.
Monitoring and Management
Posaconazole therapy necessitates careful monitoring to ensure efficacy and minimize the risk of adverse effects. This involves regular assessment of patient’s clinical condition, laboratory parameters, and potential drug interactions.
Liver Function Monitoring
Regular monitoring of liver function is crucial during posaconazole therapy, as the drug can cause hepatotoxicity. Liver function tests (LFTs), including aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), and bilirubin, should be performed before initiating treatment and periodically thereafter.
Elevated LFTs, particularly AST and ALT, may indicate liver injury.
In cases of significant LFT elevation, posaconazole therapy should be discontinued or the dosage adjusted.
Hematologic Monitoring
Posaconazole can potentially suppress bone marrow function, leading to hematologic abnormalities. Therefore, monitoring complete blood counts (CBCs) is essential.
CBCs should be performed before starting posaconazole therapy and periodically during treatment.
Specific attention should be paid to platelet counts and white blood cell (WBC) counts. If significant hematologic abnormalities are detected, posaconazole therapy may need to be adjusted or discontinued.
Managing Adverse Events
Adverse events associated with posaconazole therapy should be promptly addressed.
- Gastrointestinal disturbances, such as nausea, vomiting, and diarrhea, are common adverse effects. These can often be managed with antiemetic medications and supportive care.
- Hepatotoxicity, as discussed earlier, requires careful monitoring of LFTs and prompt discontinuation of posaconazole if significant elevations occur.
- Prolonged QT interval, a potential cardiac adverse effect, necessitates monitoring of electrocardiograms (ECGs) and appropriate management strategies.
- Hypersensitivity reactions, such as rash, itching, and angioedema, may occur. In such cases, posaconazole therapy should be discontinued and appropriate treatment initiated.
Resistance Mechanisms
Posaconazole, like other antifungal agents, faces the challenge of fungal resistance development. Understanding the mechanisms by which fungi evade the drug’s action is crucial for effective treatment and preventing the emergence of resistant strains.
Mechanisms of Resistance
Fungal resistance to posaconazole can arise through various mechanisms, including:
- Mutations in the target enzyme: Posaconazole primarily inhibits the enzyme lanosterol 14α-demethylase (CYP51), a key enzyme in ergosterol biosynthesis. Mutations in the CYP51 gene can alter the enzyme’s structure, reducing its affinity for posaconazole and hindering the drug’s ability to inhibit ergosterol production. These mutations are often observed in species like *Aspergillus fumigatus*, *Candida albicans*, and *Cryptococcus neoformans*.
- Increased efflux pump activity: Some fungi possess efflux pumps that actively expel drugs from their cells. Increased expression or activity of these pumps, such as the ABC transporter genes, can lead to reduced intracellular drug concentrations, thereby limiting the drug’s effectiveness.
- Alterations in drug metabolism: Fungi can modify posaconazole through enzymatic reactions, such as oxidation or hydroxylation, leading to inactive metabolites. These metabolic changes can decrease the drug’s bioavailability and efficacy.
- Target gene amplification: Amplification of the CYP51 gene can increase the production of the target enzyme, overcoming the inhibitory effect of posaconazole.
Impact of Resistance on Treatment Outcomes
Resistance to posaconazole can significantly impact treatment outcomes, leading to:
- Treatment failure: Resistant infections may not respond to posaconazole therapy, requiring alternative antifungal agents or combination therapy.
- Increased morbidity and mortality: Fungal infections, particularly invasive infections, can be life-threatening. Resistance can increase the risk of complications, prolonged hospital stays, and mortality.
- Emergence of multidrug resistance: Resistance to one antifungal agent can increase the likelihood of resistance to other drugs, making treatment more challenging.
Strategies for Managing Resistance
Managing resistance to posaconazole involves a multi-pronged approach:
- Appropriate drug selection: Choosing the most appropriate antifungal agent based on the infecting organism, patient factors, and susceptibility testing results is crucial.
- Optimizing drug dosage and administration: Ensuring adequate drug concentrations at the site of infection is essential for maximizing efficacy and minimizing the risk of resistance development.
- Combination therapy: Combining posaconazole with other antifungal agents with different mechanisms of action can be effective in overcoming resistance.
- Surveillance and monitoring: Regular monitoring of fungal susceptibility patterns and the emergence of resistance is crucial for informing treatment decisions and guiding public health strategies.
- Development of new antifungal agents: Research and development of new antifungal agents with novel mechanisms of action are essential to combat the challenge of resistance.
Clinical Trials and Research
Posaconazole has undergone extensive clinical trials to evaluate its efficacy and safety across various indications. Numerous studies have provided valuable insights into its clinical utility, paving the way for its widespread use in treating invasive fungal infections.
Key Findings from Clinical Trials
Clinical trials have demonstrated the effectiveness of posaconazole in treating a wide range of fungal infections, including invasive aspergillosis, mucormycosis, and candidiasis. The studies have also provided data on its safety profile, identifying potential adverse effects and establishing optimal dosing regimens.
- Invasive Aspergillosis: Posaconazole has shown efficacy in treating invasive aspergillosis, particularly in patients with hematologic malignancies and those who are immunocompromised. Studies have demonstrated its ability to improve survival rates and reduce the incidence of fungal-related mortality.
- Mucormycosis: Posaconazole has emerged as a valuable therapeutic option for mucormycosis, a severe fungal infection that often affects individuals with diabetes mellitus and those who are neutropenic. Clinical trials have shown promising results in terms of response rates and overall survival.
- Candidiasis: Posaconazole has been effective in treating various forms of candidiasis, including esophageal candidiasis, oropharyngeal candidiasis, and candidemia. Studies have demonstrated its ability to eradicate Candida species and improve clinical outcomes.
Ongoing Research and New Applications
Ongoing research efforts are exploring new applications and formulations of posaconazole, aiming to expand its therapeutic potential and address unmet clinical needs.
- New Formulations: Researchers are investigating novel formulations of posaconazole, such as liposomal and nanoparticle-based formulations, to improve its bioavailability, reduce adverse effects, and enhance its delivery to target sites. These formulations could potentially lead to more effective and convenient treatment options.
- Prophylactic Use: Studies are evaluating the potential of posaconazole for prophylactic use in high-risk patients, such as those undergoing hematopoietic stem cell transplantation or solid organ transplantation, to prevent invasive fungal infections.
- Combination Therapies: Research is exploring the efficacy of posaconazole in combination with other antifungal agents, such as echinocandins or azoles, to enhance treatment outcomes and overcome drug resistance.
Future Research Directions
Further research is needed to address several important areas related to posaconazole.
- Drug Resistance: Ongoing research is investigating the mechanisms of posaconazole resistance and exploring strategies to overcome it. Understanding the molecular basis of resistance will be crucial for developing new antifungal agents or strategies to combat it.
- Pharmacokinetic Variability: Studies are investigating the factors that influence the pharmacokinetics of posaconazole, such as age, renal function, and drug interactions. This research will contribute to optimizing dosing regimens and improving treatment outcomes.
- Safety and Toxicity: Continued research is needed to assess the long-term safety and toxicity of posaconazole, particularly in specific patient populations, such as children, pregnant women, and individuals with underlying medical conditions.
Patient Education and Counseling
It is crucial for patients to understand the importance of taking posaconazole as prescribed and to be aware of potential side effects and drug interactions. This information can help patients make informed decisions about their treatment and ensure the best possible outcomes.
Posaconazole Information for Patients
| Topic | Information |
|---|---|
| Dosage | Your doctor will determine the correct dosage of posaconazole for you based on your condition and other factors. It is important to take posaconazole exactly as prescribed. Do not skip doses or stop taking the medication without talking to your doctor. |
| Administration | Posaconazole is typically taken by mouth. It is important to take the medication with a meal to improve absorption. Avoid taking posaconazole with grapefruit juice, as it can interfere with its effectiveness. |
| Potential Side Effects | Posaconazole can cause a range of side effects, including nausea, vomiting, diarrhea, headache, and liver problems. Some side effects may be serious and require immediate medical attention. Inform your doctor about any side effects you experience. |
| Drug Interactions | Posaconazole can interact with other medications, including certain antifungal medications, immunosuppressants, and blood thinners. It is important to inform your doctor about all medications you are taking, including over-the-counter medications and herbal supplements. |
| Monitoring | Your doctor may monitor your blood levels of posaconazole to ensure that the medication is effective and safe for you. Regular blood tests and liver function tests may be required. |
Counseling Patients About Posaconazole Therapy
It is essential to provide patients with comprehensive information about posaconazole therapy. The following points can be used to guide counseling:
- Explain the purpose of posaconazole therapy and how it can help manage their condition.
- Discuss the importance of taking posaconazole as prescribed and the potential consequences of skipping doses or stopping the medication prematurely.
- Inform patients about the potential side effects of posaconazole and how to manage them. Encourage them to report any side effects to their doctor.
- Explain the importance of informing their doctor about all medications they are taking, including over-the-counter medications and herbal supplements, to avoid potential drug interactions.
- Emphasize the need for regular follow-up appointments and blood tests to monitor the effectiveness and safety of posaconazole therapy.
- Answer any questions patients may have about posaconazole therapy and provide them with written materials that summarize the information discussed.
Posaconazole emerges as a crucial weapon in the arsenal against fungal infections. Its ability to target specific fungi, coupled with its unique mechanism of action, makes it a valuable treatment option for patients battling serious fungal diseases. Understanding the nuances of posaconazole’s action, its potential side effects, and its interactions with other medications is paramount in ensuring effective and safe treatment. As research continues to explore new applications and formulations of posaconazole, the future holds promising advancements in the fight against fungal infections.
Posaconazole is an antifungal medication that’s used to treat a variety of fungal infections. It’s important to note that posaconazole can interact with other medications, so it’s crucial to inform your doctor about any other medications you’re taking, including those for conditions like angina, such as isosorbide dinitrate. Your doctor can then advise on any potential interactions and help ensure your safety while taking posaconazole.