Beta blockers side effects set the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset.
Beta blockers are a class of medications commonly prescribed to treat a variety of cardiovascular conditions, including high blood pressure, heart failure, and irregular heartbeats. They work by blocking the effects of adrenaline and other hormones on the heart, slowing down the heart rate and reducing blood pressure. While beta blockers are generally safe and effective, they can also cause a range of side effects, some of which can be serious. Understanding the potential side effects of beta blockers is crucial for patients and healthcare providers to ensure safe and effective treatment.
What are Beta Blockers?
Beta blockers are a class of medications that are commonly used to treat a variety of conditions, including high blood pressure, heart failure, and certain types of arrhythmias. They work by blocking the effects of adrenaline and noradrenaline, two hormones that can increase heart rate and blood pressure.
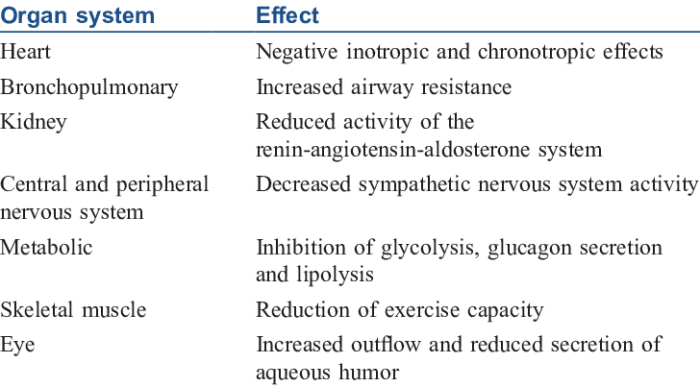
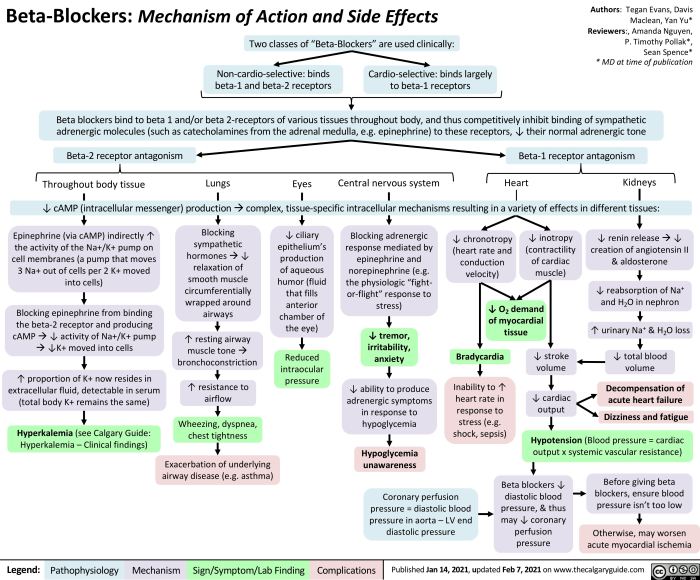
Mechanism of Action
Beta blockers work by blocking the effects of adrenaline and noradrenaline, two hormones that can increase heart rate and blood pressure. These hormones bind to beta receptors, which are found in the heart, blood vessels, and other organs. When beta blockers block these receptors, they prevent the hormones from binding and having their effects.
Types of Beta Blockers
There are two main types of beta blockers:
- Non-selective beta blockers block both beta-1 and beta-2 receptors. These are generally used for conditions that affect both the heart and the lungs, such as high blood pressure and heart failure.
- Selective beta blockers block only beta-1 receptors, which are found mainly in the heart. These are generally used for conditions that primarily affect the heart, such as high blood pressure and certain types of arrhythmias.
Common Beta Blocker Medications
The following table lists some common beta blocker medications, their brand names, and typical dosages:
| Medication | Brand Name | Typical Dosage |
|---|---|---|
| Atenolol | Tenormin | 50-100 mg daily |
| Metoprolol | Lopressor, Toprol XL | 50-200 mg daily |
| Propranolol | Inderal | 40-320 mg daily |
| Bisoprolol | Zebeta | 5-20 mg daily |
| Carvedilol | Coreg | 6.25-50 mg twice daily |
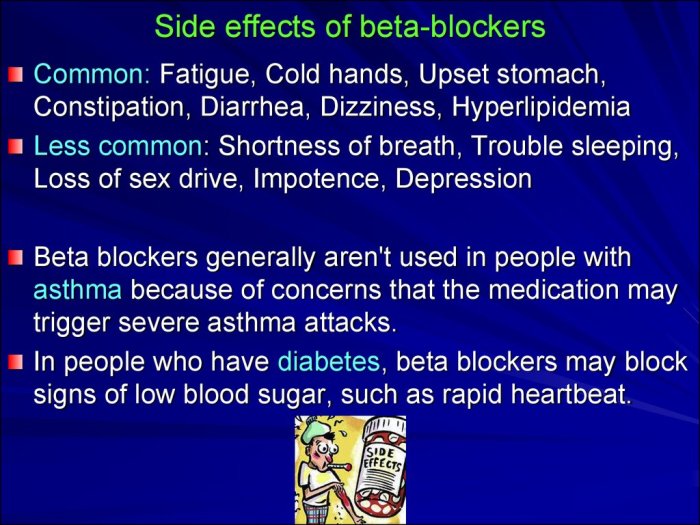
Common Side Effects of Beta Blockers
Beta blockers are a class of medications commonly prescribed to treat various cardiovascular conditions. While they are generally safe and effective, like all medications, they can cause side effects. It’s important to be aware of these potential side effects so you can discuss them with your doctor and make informed decisions about your treatment.
Cardiovascular Side Effects
Cardiovascular side effects are among the most common side effects associated with beta blockers. These medications work by blocking the effects of adrenaline (epinephrine) on the heart, which can lead to various cardiovascular changes.
- Bradycardia (Slow Heart Rate): Beta blockers slow down the heart rate, which can lead to bradycardia. This is often a mild side effect, but in some cases, it can be severe and require medical attention.
- Hypotension (Low Blood Pressure): Beta blockers can lower blood pressure, which can cause dizziness, lightheadedness, and fainting.
- Heart Failure: In rare cases, beta blockers can worsen heart failure.
- Peripheral Edema (Swelling in the Legs and Feet): Beta blockers can cause fluid retention, leading to swelling in the legs and feet.
- Cold Extremities: Beta blockers can constrict blood vessels, leading to cold hands and feet.
Respiratory Side Effects
Beta blockers can also affect the respiratory system, although these side effects are less common than cardiovascular side effects.
- Bronchospasm: Beta blockers can worsen asthma and other respiratory conditions by constricting the airways.
- Wheezing: Beta blockers can cause wheezing, especially in people with asthma.
Gastrointestinal Side Effects
Beta blockers can also affect the gastrointestinal system, leading to various side effects.
- Nausea: Beta blockers can cause nausea, which can be mild or severe.
- Vomiting: Beta blockers can also cause vomiting, which can be accompanied by nausea.
- Diarrhea: Beta blockers can cause diarrhea, which can be mild or severe.
- Constipation: Beta blockers can also cause constipation.
Other Side Effects
Beta blockers can also cause other side effects, including:
- Fatigue: Beta blockers can cause fatigue, which can be mild or severe.
- Depression: Beta blockers can also cause depression, which can be mild or severe.
- Insomnia: Beta blockers can cause insomnia, which can be mild or severe.
- Sexual Dysfunction: Beta blockers can cause sexual dysfunction, including erectile dysfunction and decreased libido.
- Dry Eyes: Beta blockers can cause dry eyes.
- Vision Changes: Beta blockers can also cause vision changes.
- Skin Reactions: Beta blockers can cause skin reactions, such as rashes, itching, and hives.
Severity and Frequency of Side Effects
The severity and frequency of side effects can vary depending on the individual, the specific beta blocker used, and the dosage. Most side effects are mild and transient, but some can be severe and require medical attention. It’s important to discuss any concerns you have with your doctor.
Serious Side Effects of Beta Blockers: Beta Blockers Side Effects
While beta blockers are generally safe and effective medications, they can cause serious side effects in some people. These side effects are rare, but it’s important to be aware of them and seek medical attention if you experience any of the symptoms.
Serious Side Effects and Risk Factors
- Slow Heart Rate (Bradycardia): Beta blockers slow down the heart rate, which can sometimes become dangerously slow. This is more likely to occur in people with pre-existing heart conditions, those taking other medications that slow the heart rate, and those with low blood pressure.
- Low Blood Pressure (Hypotension): Beta blockers can lower blood pressure, which can lead to dizziness, lightheadedness, and fainting. This is more likely to occur in people with low blood pressure, those taking other medications that lower blood pressure, and those who stand up quickly after sitting or lying down.
- Heart Failure: In some cases, beta blockers can worsen heart failure. This is more likely to occur in people with pre-existing heart failure, those with a weakened heart muscle, and those with a history of heart attack.
- Bronchospasm: Beta blockers can constrict the airways, making it difficult to breathe. This is more likely to occur in people with asthma or other lung conditions.
- Hypoglycemia: Beta blockers can mask the symptoms of low blood sugar (hypoglycemia) in people with diabetes. This is because beta blockers can prevent the body from releasing the hormones that normally raise blood sugar levels.
- Depression and Mood Changes: Beta blockers can sometimes cause depression and mood changes. This is more likely to occur in people with a history of depression.
- Sexual Dysfunction: Beta blockers can cause erectile dysfunction and other sexual problems. This is more likely to occur in men.
- Withdrawal Syndrome: Abruptly stopping beta blockers can cause a withdrawal syndrome, which can include chest pain, shortness of breath, and increased blood pressure. This is more likely to occur in people who have been taking beta blockers for a long time.
Table of Serious Side Effects
| Side Effect | Symptoms | Complications |
|---|---|---|
| Slow Heart Rate (Bradycardia) | Dizziness, lightheadedness, fainting, fatigue, shortness of breath | Cardiac arrest, heart failure |
| Low Blood Pressure (Hypotension) | Dizziness, lightheadedness, fainting, blurred vision | Falls, injuries |
| Heart Failure | Shortness of breath, fatigue, swelling in the legs and ankles | Hospitalization, death |
| Bronchospasm | Wheezing, shortness of breath, chest tightness | Respiratory failure |
| Hypoglycemia | Sweating, trembling, dizziness, confusion, headache | Seizures, coma |
| Depression and Mood Changes | Sadness, hopelessness, loss of interest in activities, fatigue, changes in sleep patterns | Suicide |
| Sexual Dysfunction | Erectile dysfunction, decreased libido | Relationship problems, depression |
| Withdrawal Syndrome | Chest pain, shortness of breath, increased blood pressure, anxiety, insomnia | Heart attack, stroke |
Managing Side Effects
Beta blockers are effective medications for treating various conditions, but they can also cause side effects. While most side effects are mild and temporary, some can be more serious. Understanding how to manage these side effects is crucial for maximizing the benefits of beta blocker therapy.
Managing Common Side Effects
Common side effects of beta blockers include fatigue, dizziness, shortness of breath, and cold hands and feet. These side effects are usually mild and often resolve within a few weeks as your body adjusts to the medication.
- Fatigue: If fatigue is bothersome, try to schedule activities for times when you have more energy. It may be helpful to get regular exercise, but avoid strenuous activities until your body adjusts to the medication.
- Dizziness: Avoid sudden movements, especially when getting up from a sitting or lying position. Sit down if you feel dizzy.
- Shortness of Breath: If shortness of breath is a concern, talk to your doctor. They may adjust your dosage or recommend lifestyle changes, such as quitting smoking or losing weight.
- Cold Hands and Feet: Wear warm clothing, especially in cold weather. Avoid smoking and caffeine, which can worsen cold extremities.
Minimizing the Risk of Serious Side Effects
While serious side effects from beta blockers are uncommon, it’s essential to be aware of potential risks. These include a slow heart rate, low blood pressure, and worsening asthma symptoms.
- Slow Heart Rate: If you experience a slow heart rate, it’s crucial to seek medical attention immediately.
- Low Blood Pressure: Monitor your blood pressure regularly, especially when starting beta blocker therapy. If your blood pressure is too low, your doctor may adjust your dosage or recommend lifestyle changes, such as increasing salt intake or staying hydrated.
- Worsening Asthma Symptoms: If you have asthma, it’s important to talk to your doctor about the risks and benefits of beta blockers before starting treatment.
Interventions for Specific Side Effects
| Side Effect | Potential Interventions |
|---|---|
| Fatigue | Adjust dosage, consider changing medication, get regular exercise, avoid strenuous activities. |
| Dizziness | Adjust dosage, avoid sudden movements, sit down if you feel dizzy. |
| Shortness of Breath | Adjust dosage, consider changing medication, quit smoking, lose weight. |
| Cold Hands and Feet | Wear warm clothing, avoid smoking and caffeine. |
| Slow Heart Rate | Adjust dosage, consider changing medication, seek medical attention if symptoms worsen. |
| Low Blood Pressure | Adjust dosage, consider changing medication, increase salt intake, stay hydrated. |
| Worsening Asthma Symptoms | Consider changing medication, discuss with your doctor before starting beta blockers. |
Interactions with Other Medications
Beta blockers can interact with other medications, sometimes leading to serious consequences. Understanding these interactions is crucial for safe and effective treatment. It’s important to inform your doctor about all the medications you’re taking, including over-the-counter drugs, herbal supplements, and vitamins.
Common Medications that Interact with Beta Blockers
Interactions between beta blockers and other medications can occur due to similar mechanisms of action or competition for the same metabolic pathways. This can lead to increased or decreased effects of either medication, or even the development of new side effects.
- Calcium Channel Blockers: These medications, used for high blood pressure and heart conditions, can enhance the effects of beta blockers, leading to a significant drop in blood pressure.
- Digoxin: This medication, used for heart failure, can accumulate in the body when taken with beta blockers, increasing the risk of toxicity.
- Insulin and Oral Diabetes Medications: Beta blockers can mask the symptoms of low blood sugar (hypoglycemia) in people with diabetes, making it difficult to recognize and treat.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs, commonly used for pain and inflammation, can reduce the effectiveness of beta blockers.
- Antidepressants: Some antidepressants, particularly monoamine oxidase inhibitors (MAOIs), can interact with beta blockers, potentially leading to increased blood pressure or heart rate.
Potential Consequences of Interactions
The potential consequences of drug interactions with beta blockers can vary depending on the specific medications involved and the individual’s health status. Here’s a table illustrating common interactions, their potential outcomes, and recommended precautions:
| Medication | Potential Outcome | Precautions |
|---|---|---|
| Calcium Channel Blockers | Increased risk of low blood pressure, dizziness, and fainting | Monitor blood pressure closely, adjust dosage as needed |
| Digoxin | Increased risk of digoxin toxicity, leading to irregular heartbeat, nausea, and vomiting | Monitor digoxin levels regularly, adjust dosage as needed |
| Insulin and Oral Diabetes Medications | Masking of hypoglycemia symptoms, leading to delayed treatment and potential complications | Monitor blood sugar closely, adjust dosage as needed |
| Nonsteroidal Anti-inflammatory Drugs (NSAIDs) | Reduced effectiveness of beta blockers in lowering blood pressure and heart rate | Use alternative pain relievers if possible, consider alternative beta blocker if needed |
| Antidepressants (MAOIs) | Increased risk of high blood pressure and heart rate | Avoid use of MAOIs with beta blockers, consider alternative antidepressants |
Beta Blockers and Specific Conditions
Beta blockers are commonly used to treat various medical conditions, including high blood pressure, heart disease, and migraines. However, their use in patients with specific conditions like asthma, diabetes, or heart failure requires careful consideration due to potential interactions and risks.
Beta Blockers and Asthma
Beta blockers can worsen asthma symptoms by blocking the effects of beta-2 receptors in the lungs, which are responsible for bronchodilation. This can lead to bronchospasm, making breathing difficult. However, some beta blockers, such as atenolol and metoprolol, have a lower affinity for beta-2 receptors and may be safer for patients with asthma.
Beta Blockers and Diabetes
Beta blockers can mask the symptoms of hypoglycemia (low blood sugar) in people with diabetes, making it harder to recognize and treat. They can also interfere with the body’s ability to produce glucose, potentially leading to hypoglycemia. For this reason, it’s crucial to monitor blood sugar levels closely and adjust insulin or oral medication doses as needed when taking beta blockers.
Beta Blockers and Heart Failure
Beta blockers can be beneficial for some patients with heart failure, particularly those with a reduced ejection fraction (the amount of blood pumped out of the heart with each beat). They can help improve heart function, reduce symptoms, and lower the risk of death. However, beta blockers should be used with caution in patients with severe heart failure, as they can worsen symptoms in some cases.
Considerations for Dosage and Monitoring
| Condition | Dosage | Monitoring |
|---|---|---|
| Asthma | Start with a low dose and increase gradually as tolerated. Consider beta blockers with lower affinity for beta-2 receptors. | Monitor for signs of bronchospasm, such as wheezing, shortness of breath, and chest tightness. |
| Diabetes | Start with a low dose and monitor blood sugar levels closely. Adjust insulin or oral medication doses as needed. | Monitor blood sugar levels regularly, especially during the first few weeks of treatment. |
| Heart Failure | Start with a low dose and increase gradually as tolerated. Monitor for signs of worsening heart failure, such as fatigue, shortness of breath, and swelling in the legs and ankles. | Monitor heart function, blood pressure, and electrolyte levels regularly. |
Beta Blockers and Pregnancy
Beta blockers are a class of medications commonly used to treat various conditions, including high blood pressure, heart rhythm problems, and migraines. However, their use during pregnancy and breastfeeding requires careful consideration due to potential risks and benefits.
Pregnancy and breastfeeding are unique physiological states that can affect how medications are absorbed, distributed, metabolized, and eliminated. Beta blockers can cross the placenta and enter the fetal circulation, potentially impacting fetal development. Similarly, they can be transferred to the infant through breast milk, potentially affecting the infant’s health.
Safety Profile of Beta Blockers During Pregnancy and Lactation
The safety profile of beta blockers during pregnancy and lactation varies depending on the specific medication and the stage of pregnancy. Some beta blockers, such as atenolol and metoprolol, are considered relatively safe for use during pregnancy, while others, such as propranolol, are associated with a higher risk of fetal complications.
Here’s a table summarizing the safety profile of different beta blockers during pregnancy and lactation:
| Beta Blocker | Pregnancy Category | Lactation | Comments |
|—|—|—|—|
| Atenolol | C | Compatible | May be used during pregnancy and lactation with careful monitoring. |
| Metoprolol | C | Compatible | May be used during pregnancy and lactation with careful monitoring. |
| Propranolol | D | Compatible | Avoid use during pregnancy unless benefits outweigh risks. May be used during lactation with caution. |
| Bisoprolol | C | Compatible | May be used during pregnancy and lactation with careful monitoring. |
| Carvedilol | C | Compatible | May be used during pregnancy and lactation with careful monitoring. |
It’s crucial to consult with a healthcare professional before taking any beta blocker during pregnancy or breastfeeding. They can assess the potential risks and benefits, weigh them against the mother’s and fetus’s individual needs, and recommend the most appropriate treatment plan.
Beta Blockers and Lifestyle Factors
Lifestyle factors play a significant role in how your body responds to beta blockers. Certain lifestyle choices can either enhance or hinder the effectiveness of these medications. Understanding these interactions is crucial for optimizing your treatment plan and achieving the best possible outcomes.
Lifestyle Factors and Beta Blocker Effects
Lifestyle modifications can have a considerable impact on the efficacy and side effects of beta blockers. Making positive changes to your diet, exercise routine, and alcohol consumption can help manage side effects and improve the effectiveness of your medication.
Diet
- Reduce Sodium Intake: High sodium intake can worsen fluid retention and increase blood pressure, which can counteract the effects of beta blockers. Aim to limit your sodium intake to 2,300 milligrams per day or less.
- Increase Potassium Intake: Beta blockers can deplete potassium levels, which can lead to irregular heartbeats. Increasing potassium-rich foods in your diet, such as bananas, potatoes, and leafy greens, can help maintain healthy potassium levels.
- Limit Caffeine: Caffeine can interfere with the effectiveness of beta blockers by increasing heart rate and blood pressure. Limit your caffeine intake to 200-400 milligrams per day, equivalent to 2-4 cups of coffee.
- Maintain a Healthy Weight: Obesity can increase blood pressure and strain your heart, making beta blockers less effective. Losing weight can improve your overall health and enhance the effects of your medication.
Exercise
- Regular Exercise: Regular physical activity can improve heart health and enhance the effects of beta blockers. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Avoid Overexertion: Beta blockers can reduce your heart’s ability to respond to physical exertion. Avoid strenuous activities that may cause shortness of breath or chest pain. Consult with your doctor about appropriate exercise levels for your individual needs.
Alcohol Consumption
- Moderate Alcohol Consumption: Excessive alcohol intake can interfere with the effectiveness of beta blockers and increase the risk of side effects. Limit your alcohol consumption to one drink per day for women and two drinks per day for men.
Table of Lifestyle Changes and Their Potential Impact, Beta blockers side effects
| Lifestyle Change | Potential Impact on Beta Blocker Efficacy | Potential Impact on Side Effects |
|---|---|---|
| Reduced Sodium Intake | Improved blood pressure control, enhancing effectiveness | Reduced fluid retention, minimizing swelling |
| Increased Potassium Intake | Improved heart rhythm, enhancing effectiveness | Reduced risk of irregular heartbeats |
| Limited Caffeine Intake | Improved heart rate control, enhancing effectiveness | Reduced anxiety, tremors, and insomnia |
| Healthy Weight Maintenance | Improved overall heart health, enhancing effectiveness | Reduced blood pressure, improving overall health |
| Regular Exercise | Improved cardiovascular health, enhancing effectiveness | Reduced risk of heart disease and stroke |
| Moderate Alcohol Consumption | Minimized interference with medication efficacy | Reduced risk of side effects |
Navigating the world of beta blockers requires a careful balance between their potential benefits and the risks associated with their side effects. Understanding the common and serious side effects, managing them effectively, and staying informed about potential interactions with other medications are crucial steps in ensuring a safe and successful treatment journey. By working closely with your healthcare provider, you can make informed decisions about your treatment plan and minimize the risk of adverse effects.
Beta blockers can sometimes cause side effects like fatigue and low blood sugar, which is why it’s important to be aware of these potential issues. If you’re taking a beta blocker and experience these symptoms, it’s crucial to consult your doctor. They might recommend adjusting your medication or exploring alternative treatment options, such as using a different type of insulin like basaglar insulin , which might be better suited for your needs.
Remember, your doctor is your best resource for managing any potential side effects from medications.