Neomycin and polymyxin B sulfates are a potent antibiotic duo frequently employed in the fight against bacterial infections. These medications, often administered topically or orally, are known for their broad-spectrum activity against a wide range of bacteria, including Gram-positive and Gram-negative species. Their unique mechanisms of action and pharmacological properties make them valuable tools in the treatment of various infections, from skin and eye infections to gastrointestinal disturbances.
The combination of neomycin and polymyxin B sulfates offers a synergistic approach to combating bacterial infections. Neomycin, an aminoglycoside antibiotic, inhibits bacterial protein synthesis, while polymyxin B, a polypeptide antibiotic, disrupts bacterial cell membranes. This combined action effectively targets multiple aspects of bacterial survival, enhancing their overall effectiveness against susceptible bacteria.
Neomycin and Polymyxin B Sulfates
Neomycin and polymyxin B sulfates are two antibiotics commonly used in combination to treat various bacterial infections, particularly those affecting the skin and eyes. These antibiotics work synergistically, meaning they enhance each other’s effectiveness, making them a potent treatment option.
Chemical Structures of Neomycin and Polymyxin B Sulfates
Neomycin and polymyxin B sulfates are structurally distinct antibiotics with different chemical compositions.
Neomycin is an aminoglycoside antibiotic derived from the bacterium *Streptomyces fradiae*. Its chemical structure is characterized by a complex sugar molecule with multiple amino groups attached.
Polymyxin B is a polypeptide antibiotic produced by the bacterium *Bacillus polymyxa*. Its structure consists of a cyclic peptide chain with a fatty acid tail. The sulfate form of polymyxin B, polymyxin B sulfate, is commonly used in medical applications.
Mechanism of Action
Both neomycin and polymyxin B sulfates exert their antimicrobial effects by targeting different bacterial components.
Neomycin
Neomycin’s mechanism of action involves interfering with bacterial protein synthesis. It binds to the 30S ribosomal subunit of bacteria, disrupting the translation process and preventing the formation of functional proteins. This ultimately leads to bacterial cell death.
Polymyxin B Sulfates
Polymyxin B sulfates, on the other hand, disrupt bacterial cell membranes. They bind to the lipopolysaccharide (LPS) layer of the outer membrane of gram-negative bacteria. This binding disrupts the membrane’s integrity, leading to leakage of essential cellular components and ultimately bacterial cell death.
Pharmacological Properties
Neomycin
- Neomycin is primarily used topically, applied directly to the skin or eyes, due to its poor oral absorption and potential for toxicity.
- It is effective against a broad spectrum of gram-positive and gram-negative bacteria, including *Staphylococcus aureus*, *Streptococcus pyogenes*, and *Escherichia coli*.
- Neomycin can cause local irritation, redness, and itching when applied topically.
- Systemic absorption of neomycin can lead to ototoxicity (hearing loss) and nephrotoxicity (kidney damage), especially in individuals with pre-existing kidney or hearing problems.
Polymyxin B Sulfates
- Polymyxin B sulfates are also primarily used topically, although they can be administered intravenously in severe cases of gram-negative bacterial infections.
- They are effective against a wide range of gram-negative bacteria, including *Pseudomonas aeruginosa*, *Acinetobacter baumannii*, and *Klebsiella pneumoniae*.
- Polymyxin B sulfates can cause local irritation and hypersensitivity reactions when applied topically.
- Intravenous administration of polymyxin B sulfates can lead to nephrotoxicity and neurotoxicity, including seizures and coma.
Spectrum of Activity

Neomycin and polymyxin B sulfates are antibiotics that exhibit a broad spectrum of activity against various bacterial species. Their effectiveness against Gram-positive and Gram-negative bacteria varies, making it crucial to understand their specific actions for optimal therapeutic use.
Susceptible Bacterial Species
Neomycin and polymyxin B sulfates are effective against a wide range of bacteria, including both Gram-positive and Gram-negative species.
- Gram-positive bacteria: Neomycin is generally more effective against Gram-positive bacteria, including Staphylococcus aureus, Streptococcus pyogenes, and Enterococcus faecalis. Polymyxin B sulfates, on the other hand, have limited activity against Gram-positive bacteria.
- Gram-negative bacteria: Polymyxin B sulfates are highly effective against Gram-negative bacteria, particularly Pseudomonas aeruginosa and Escherichia coli. Neomycin also demonstrates some activity against Gram-negative bacteria but is less potent than polymyxin B sulfates.
Effectiveness Against Gram-Positive and Gram-Negative Bacteria
The effectiveness of neomycin and polymyxin B sulfates against Gram-positive and Gram-negative bacteria is influenced by their unique mechanisms of action.
- Neomycin: This antibiotic inhibits protein synthesis by binding to the 30S ribosomal subunit, preventing the formation of functional ribosomes. This mechanism is effective against both Gram-positive and Gram-negative bacteria, although its activity against Gram-negative bacteria is generally weaker due to the presence of an outer membrane that acts as a barrier.
- Polymyxin B sulfates: These antibiotics target the bacterial cell membrane, disrupting its integrity and leading to cell death. Polymyxin B sulfates are particularly effective against Gram-negative bacteria because they can penetrate their outer membrane more readily than neomycin. Their activity against Gram-positive bacteria is limited due to the lack of an outer membrane.
Activity Against Specific Pathogens
Neomycin and polymyxin B sulfates exhibit specific activity against certain pathogens.
Pseudomonas aeruginosa
Polymyxin B sulfates are highly effective against Pseudomonas aeruginosa, a Gram-negative bacterium known for its resistance to many antibiotics. This effectiveness stems from its ability to penetrate the outer membrane of Pseudomonas aeruginosa and disrupt its cell membrane. Neomycin, while exhibiting some activity against Pseudomonas aeruginosa, is less potent than polymyxin B sulfates.
Escherichia coli
Both neomycin and polymyxin B sulfates are effective against Escherichia coli, a common Gram-negative bacterium. Polymyxin B sulfates are generally preferred due to their higher potency and ability to penetrate the outer membrane of Escherichia coli. However, neomycin can also be effective in certain cases, particularly when combined with other antibiotics.
Pharmacokinetics: Neomycin And Polymyxin B Sulfates
The pharmacokinetic profile of neomycin and polymyxin B sulfates refers to their movement within the body, including absorption, distribution, metabolism, and excretion. Understanding these processes is crucial for determining optimal dosage, potential side effects, and drug interactions.
Absorption
The absorption of neomycin and polymyxin B sulfates depends primarily on the route of administration.
- Oral Administration: Neomycin and polymyxin B sulfates are poorly absorbed from the gastrointestinal tract. This is because they are large, polar molecules that are not readily transported across the intestinal lining.
- Topical Administration: When applied topically, neomycin and polymyxin B sulfates are absorbed to a limited extent through the skin. The extent of absorption can vary depending on the integrity of the skin barrier and the presence of any underlying inflammation or wounds.
- Intramuscular Administration: Neomycin and polymyxin B sulfates are not typically administered intramuscularly due to their potential for toxicity. However, in rare cases, they may be used intramuscularly for specific indications, such as severe infections.
Distribution
Once absorbed, neomycin and polymyxin B sulfates distribute throughout the body, primarily to the kidneys, liver, and lungs. However, they do not readily cross the blood-brain barrier, meaning their concentration in the central nervous system is typically low.
Metabolism
Neomycin and polymyxin B sulfates are not significantly metabolized in the body. They are primarily excreted unchanged in the urine.
Excretion
Neomycin and polymyxin B sulfates are primarily excreted through the kidneys in the urine. The rate of excretion can vary depending on renal function.
Factors Influencing Pharmacokinetics
Several factors can influence the pharmacokinetic profile of neomycin and polymyxin B sulfates, including:
- Route of Administration: As mentioned earlier, the route of administration significantly impacts absorption and distribution. Oral administration results in minimal absorption, while topical administration leads to limited absorption through the skin.
- Renal Function: Impaired renal function can significantly affect the excretion of neomycin and polymyxin B sulfates, leading to their accumulation in the body and an increased risk of toxicity.
- Patient Factors: Factors such as age, body weight, and overall health status can also influence pharmacokinetics. For example, infants and elderly individuals may have altered drug metabolism and excretion, potentially requiring dosage adjustments.
| Pharmacokinetic Parameter | Neomycin | Polymyxin B Sulfates |
|---|---|---|
| Absorption | Poorly absorbed orally, limited absorption topically | Poorly absorbed orally, limited absorption topically |
| Distribution | Distributes to kidneys, liver, and lungs; does not readily cross the blood-brain barrier | Distributes to kidneys, liver, and lungs; does not readily cross the blood-brain barrier |
| Metabolism | Not significantly metabolized | Not significantly metabolized |
| Excretion | Primarily excreted in urine | Primarily excreted in urine |
Clinical Applications

Neomycin and polymyxin B sulfates, as a combination, have established themselves as valuable therapeutic agents in various clinical settings. Their synergistic action against a wide range of bacterial species makes them effective in treating a variety of infections.
Skin Infections
The topical application of neomycin and polymyxin B sulfates is frequently employed in the management of skin infections. These antibiotics are particularly effective against gram-negative bacteria, which are common culprits in skin infections.
- Dermatitis: Neomycin and polymyxin B sulfates are often prescribed for the treatment of dermatitis, a common skin condition characterized by inflammation and irritation.
- Impetigo: This contagious bacterial skin infection is often treated with topical neomycin and polymyxin B sulfates, particularly in cases caused by Staphylococcus aureus or Streptococcus pyogenes.
- Wound infections: These antibiotics are also useful in preventing and treating wound infections, especially those caused by gram-negative bacteria.
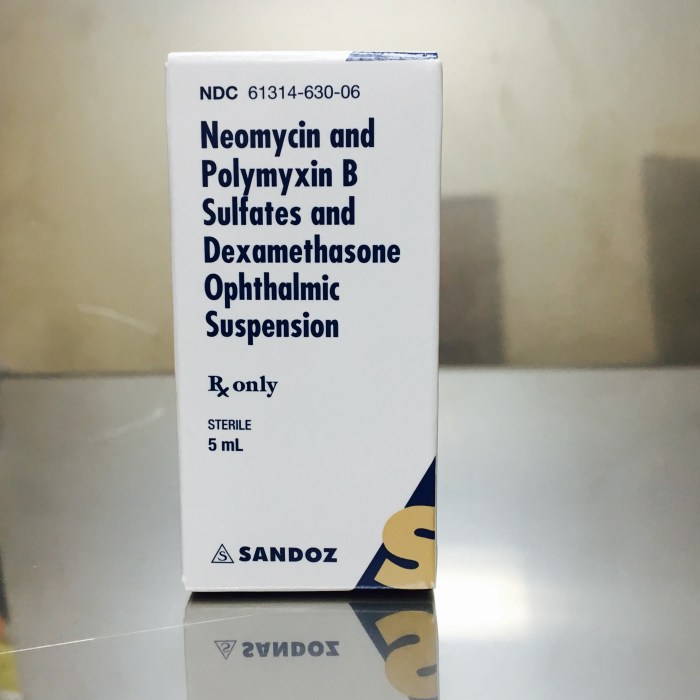
Eye Infections
Ophthalmic preparations of neomycin and polymyxin B sulfates are commonly used to treat bacterial conjunctivitis, also known as “pink eye.”
- Conjunctivitis: This infection, characterized by redness, swelling, and discharge in the conjunctiva (the clear membrane covering the white part of the eye), is often caused by bacteria. Neomycin and polymyxin B sulfates are effective against a wide range of bacterial species that commonly cause conjunctivitis.
Gastrointestinal Infections
Neomycin and polymyxin B sulfates are used in certain gastrointestinal infections, particularly those caused by gram-negative bacteria.
- Hepatic encephalopathy: This condition, characterized by brain dysfunction due to liver failure, is often treated with neomycin. The antibiotic helps reduce the production of ammonia in the gut, which can contribute to the development of hepatic encephalopathy.
- Preoperative bowel preparation: Neomycin is sometimes used to sterilize the bowel before surgery, particularly in patients undergoing procedures that involve the gastrointestinal tract.
Other Applications
Neomycin and polymyxin B sulfates are also used in other clinical settings, including:
- Otitis externa: This infection of the outer ear canal is often treated with topical neomycin and polymyxin B sulfates.
- Prophylaxis: These antibiotics can be used to prevent infections in certain high-risk individuals, such as those undergoing surgery or with weakened immune systems.
Adverse Effects and Drug Interactions
Neomycin and polymyxin B sulfates, while effective antibiotics, can cause various adverse effects, some of which can be serious. These effects are primarily due to their mechanisms of action, which involve disrupting bacterial cell membranes and interfering with protein synthesis. Understanding these adverse effects is crucial for safe and effective use of these antibiotics.
Adverse Effects
Adverse effects of neomycin and polymyxin B sulfates are categorized based on their severity and organ systems affected.
- Gastrointestinal Effects: These are the most common adverse effects, particularly with neomycin. They include nausea, vomiting, diarrhea, and abdominal cramps. These effects occur due to the disruption of normal gut flora by the antibiotics, leading to an imbalance in the intestinal microbiome.
- Neurotoxicity: Both neomycin and polymyxin B sulfates can cause neurotoxicity, especially with high doses or prolonged use. This can manifest as dizziness, confusion, tremors, seizures, and even coma. The mechanism involves the accumulation of these antibiotics in the central nervous system, interfering with nerve function.
- Nephrotoxicity: Both antibiotics can damage the kidneys, particularly in individuals with pre-existing kidney disease or those receiving high doses. This can lead to a decrease in urine output, elevated blood creatinine levels, and even kidney failure. The mechanism involves the direct toxicity of these antibiotics to the renal tubules.
- Ototoxicity: Neomycin is known to cause ototoxicity, which can affect both hearing and balance. This can manifest as tinnitus, hearing loss, and vertigo. The mechanism involves damage to the hair cells in the inner ear, which are responsible for hearing and balance.
- Hypersensitivity Reactions: Allergic reactions to neomycin and polymyxin B sulfates are possible, though less common. These reactions can range from mild skin rashes to severe anaphylaxis. The mechanism involves the immune system’s response to the antibiotics, leading to the release of histamine and other inflammatory mediators.
Drug Interactions
The potential for drug interactions with neomycin and polymyxin B sulfates is significant, as they can affect the absorption, metabolism, and excretion of other medications.
- Increased Risk of Nephrotoxicity: When used concurrently with other nephrotoxic drugs, such as aminoglycosides (e.g., gentamicin, tobramycin), loop diuretics (e.g., furosemide, bumetanide), or NSAIDs (e.g., ibuprofen, naproxen), the risk of kidney damage is increased. This is due to the additive effects of these drugs on the kidneys.
- Reduced Effectiveness of Other Antibiotics: Neomycin and polymyxin B sulfates can interfere with the effectiveness of other antibiotics, particularly those that target bacterial cell walls (e.g., penicillin, cephalosporins). This occurs because these antibiotics can disrupt the bacterial cell membrane, making it harder for other antibiotics to penetrate and exert their effects.
- Altered Absorption of Other Drugs: Neomycin can interfere with the absorption of other medications, particularly those that are absorbed in the small intestine. This is due to the antibiotic’s ability to bind to and inactivate certain drugs. For example, neomycin can reduce the absorption of digoxin, a heart medication.
- Increased Risk of Ototoxicity: The risk of ototoxicity is increased when neomycin is used concurrently with other ototoxic drugs, such as loop diuretics (e.g., furosemide, bumetanide) or certain chemotherapy drugs (e.g., cisplatin). This is due to the additive effects of these drugs on the inner ear.
Dosage and Administration
The dosage of neomycin and polymyxin B sulfates varies depending on the indication, route of administration, and patient factors. It’s crucial to consult a healthcare professional for appropriate dosage and administration guidelines.
Recommended Dosage Regimens
Dosage regimens for neomycin and polymyxin B sulfates are tailored based on the specific condition being treated. The following table provides a general overview of dosage ranges for common applications:
| Indication | Dosage Form | Route of Administration | Typical Dosage Range |
|---|---|---|---|
| Otic Infections | Otic solution | Topical (ear drops) | 3-5 drops in the affected ear 3-4 times daily |
| Ophthalmic Infections | Ophthalmic solution | Topical (eye drops) | 1-2 drops in the affected eye 3-4 times daily |
| Skin Infections | Cream, ointment | Topical | Apply a thin layer to the affected area 2-4 times daily |
Routes of Administration, Neomycin and polymyxin b sulfates
Neomycin and polymyxin B sulfates are primarily administered topically, but can also be used intravenously in specific circumstances.
- Topical Administration: This is the most common route of administration for neomycin and polymyxin B sulfates, used for treating skin, ear, and eye infections.
- Intravenous Administration: In rare cases, neomycin and polymyxin B sulfates can be administered intravenously for severe systemic infections. This route is typically reserved for patients with life-threatening conditions and is administered under strict medical supervision.
Resistance and Resistance Mechanisms
While neomycin and polymyxin B sulfates have historically been effective against a wide range of bacteria, the emergence of resistance is a growing concern. This resistance can significantly impact the efficacy of these antibiotics, posing challenges for treating infections.
Mechanisms of Resistance
Resistance to neomycin and polymyxin B sulfates can arise through various mechanisms, including mutations in target sites and enzymatic inactivation.
Mutations in Target Sites
Mutations in the target sites of these antibiotics are a primary mechanism of resistance. For neomycin, the target is the 16S rRNA component of the 30S ribosomal subunit, crucial for protein synthesis. Mutations in this region can disrupt the binding of neomycin, rendering the bacteria resistant.
Polymyxin B, on the other hand, targets the lipopolysaccharide (LPS) layer of the bacterial outer membrane. Mutations in the LPS structure, particularly in the lipid A component, can reduce the affinity of polymyxin B for the bacterial cell wall, leading to resistance.
Enzymatic Inactivation
Another mechanism of resistance involves the production of enzymes that inactivate the antibiotic. Neomycin can be inactivated by aminoglycoside-modifying enzymes (AMEs), which add chemical groups to the antibiotic molecule, altering its structure and preventing its binding to the ribosome.
Similarly, polymyxin B can be inactivated by enzymes that modify the lipid A component of LPS, reducing its susceptibility to the antibiotic. These enzymes can be acquired through horizontal gene transfer, allowing resistance to spread rapidly among bacterial populations.
Implications of Resistance
The emergence of resistance to neomycin and polymyxin B sulfates has significant implications for clinical practice and infection control.
Clinical Practice
Resistant strains can cause treatment failures, requiring alternative therapies that may be less effective or have more adverse effects. Infections caused by resistant strains can also be more difficult to manage and may require prolonged hospitalization.
Infection Control
The spread of resistant strains poses a significant challenge for infection control measures. These strains can easily transmit between individuals, leading to outbreaks in healthcare settings.
Furthermore, the overuse and misuse of these antibiotics can contribute to the selection and spread of resistant strains. Prudent use of antibiotics, including appropriate dosing and duration of treatment, is crucial for preventing the emergence and spread of resistance.
Future Directions
Neomycin and polymyxin B sulfates have been valuable antibiotics for decades, but their effectiveness is threatened by increasing resistance and emerging challenges. Ongoing research aims to address these issues and explore new applications for these agents.
Strategies to Overcome Resistance
The development of resistance to neomycin and polymyxin B sulfates is a significant concern. Research efforts are focused on developing strategies to overcome resistance and enhance therapeutic efficacy.
- Combination Therapy: Combining neomycin or polymyxin B with other antibiotics with different mechanisms of action can potentially circumvent resistance. This strategy can prevent the emergence of resistant strains and improve therapeutic outcomes.
- Novel Drug Delivery Systems: Encapsulation of neomycin or polymyxin B within nanoparticles or liposomes can enhance drug delivery to the target site, potentially increasing their efficacy and reducing side effects. This approach can also protect the antibiotics from degradation and enhance their stability.
- Targeting Resistance Mechanisms: Research is ongoing to identify and target the specific mechanisms of resistance to neomycin and polymyxin B. This could involve developing new drugs that circumvent resistance pathways or modifying existing antibiotics to overcome resistance mechanisms.
The use of neomycin and polymyxin B sulfates is a testament to the ongoing advancements in antimicrobial therapy. While their efficacy against various infections is undeniable, it is crucial to be mindful of the potential adverse effects and the emergence of bacterial resistance. Continued research into optimizing their use and developing novel strategies to combat resistance will ensure their continued role in safeguarding human health against infectious diseases.
Neomycin and polymyxin B sulfates are often used together in topical medications to combat bacterial infections. While these medications target bacteria directly, it’s important to note that conditions like edema, which can sometimes accompany infection, may require a different approach. In such cases, a diuretic like furosemide 20 mg could be prescribed to reduce fluid buildup. However, it’s crucial to remember that neomycin and polymyxin B sulfates are only effective against bacterial infections and do not address underlying conditions like edema.