Amikacin, a potent aminoglycoside antibiotic, stands as a vital weapon in the fight against severe bacterial infections. Its unique chemical structure and mechanism of action enable it to target a wide range of bacteria, making it a valuable tool for clinicians treating life-threatening conditions. Since its introduction in the 1970s, amikacin has played a critical role in managing infections that are resistant to other antibiotics.
This comprehensive review delves into the intricacies of amikacin, exploring its pharmacokinetic properties, clinical applications, and potential adverse effects. We will also examine the emerging challenges of bacterial resistance and discuss future research directions aimed at optimizing amikacin’s therapeutic efficacy.
Amikacin

Amikacin is a potent aminoglycoside antibiotic used to treat serious bacterial infections, particularly those caused by gram-negative bacteria. Its effectiveness against a wide range of bacteria makes it a valuable tool in the fight against infections, especially in situations where other antibiotics have failed.
Chemical Structure and Properties
Amikacin is a complex molecule composed of a 2-deoxystreptamine nucleus linked to various sugar moieties. Its chemical formula is C22H43N5O13, and it has a molecular weight of 585.6 g/mol. Amikacin is a white to off-white crystalline powder that is soluble in water. Its chemical structure is characterized by the presence of several amino groups, which are responsible for its antibiotic activity.
Mechanism of Action
Amikacin exerts its antibacterial effect by inhibiting protein synthesis in bacteria. It binds to the 30S ribosomal subunit of bacterial ribosomes, preventing the formation of the initiation complex required for translation. This interference with protein synthesis leads to the death of the bacterial cell.
History of Development and Approval
Amikacin was first synthesized in the 1970s by researchers at Bristol-Myers Squibb. The drug was developed as a semisynthetic derivative of kanamycin, another aminoglycoside antibiotic. Amikacin was designed to overcome the resistance that had developed to kanamycin and other aminoglycosides. After extensive clinical trials, amikacin was approved by the Food and Drug Administration (FDA) in 1978 for the treatment of serious bacterial infections.
Pharmacokinetics of Amikacin
Amikacin, like other aminoglycosides, exhibits a complex pharmacokinetic profile, influenced by various factors. Understanding these properties is crucial for optimizing its therapeutic efficacy and minimizing potential adverse effects.
Absorption
Amikacin is administered intravenously or intramuscularly, bypassing the first-pass metabolism and ensuring rapid entry into the systemic circulation. Intravenous administration offers faster and more predictable absorption compared to intramuscular injection, which may be affected by factors like injection site and blood flow.
Distribution
Amikacin distributes widely in the body, reaching therapeutic concentrations in various tissues and fluids, including the lungs, kidneys, and pleural fluid. However, it poorly penetrates the central nervous system due to its hydrophilic nature and limited crossing of the blood-brain barrier. The distribution volume is relatively small, indicating limited tissue penetration and primarily extracellular distribution.
Metabolism
Amikacin is minimally metabolized in the body, with less than 10% undergoing enzymatic degradation. Its stability allows for prolonged therapeutic effects, reducing the need for frequent dosing.
Excretion
Amikacin is primarily excreted unchanged by the kidneys through glomerular filtration. Renal function significantly influences its elimination, with impaired renal function leading to prolonged half-life and increased risk of toxicity.
Factors Influencing Amikacin Pharmacokinetics
Several factors can influence amikacin pharmacokinetics, affecting its therapeutic efficacy and safety:
- Renal Function: Amikacin’s elimination primarily depends on renal function. Reduced glomerular filtration rate prolongs its half-life, increasing the risk of toxicity.
- Age: Elderly patients often have reduced renal function, leading to slower elimination and increased drug accumulation.
- Inflammatory Conditions: Inflammation can alter tissue perfusion and drug distribution, potentially affecting amikacin’s therapeutic efficacy.
- Dosage and Frequency: Higher doses and more frequent administration can lead to higher peak concentrations, increasing the risk of toxicity.
- Drug Interactions: Co-administration with other nephrotoxic drugs can increase the risk of renal impairment.
Comparison with Other Aminoglycosides
Amikacin shares similar pharmacokinetic properties with other aminoglycosides, such as gentamicin and tobramycin. All are administered intravenously or intramuscularly, exhibit minimal metabolism, and are primarily excreted by the kidneys. However, amikacin exhibits a longer half-life compared to gentamicin and tobramycin, requiring less frequent dosing. This longer half-life also contributes to its resistance to enzymatic inactivation, making it effective against some aminoglycoside-resistant strains of bacteria.
Clinical Uses of Amikacin
Amikacin is a broad-spectrum aminoglycoside antibiotic used to treat various serious bacterial infections, particularly those resistant to other antibiotics. It is effective against a wide range of gram-negative bacteria, including Pseudomonas aeruginosa, Acinetobacter baumannii, and Enterobacteriaceae.
Primary Indications for Amikacin Therapy
Amikacin is primarily indicated for the treatment of serious infections caused by susceptible gram-negative bacteria. These infections can affect various parts of the body, including the lungs, urinary tract, skin, and bloodstream. Specific indications include:
- Hospital-acquired pneumonia: Amikacin is often used to treat pneumonia that develops in hospitalized patients, particularly those with multidrug-resistant bacteria.
- Sepsis: Amikacin is a valuable treatment option for sepsis, a life-threatening condition caused by the body’s response to infection.
- Urinary tract infections: Amikacin can be used to treat severe or complicated urinary tract infections, especially those caused by resistant bacteria.
- Skin and soft tissue infections: Amikacin is effective against certain skin and soft tissue infections, particularly those caused by Pseudomonas aeruginosa.
- Endocarditis: Amikacin may be used in combination with other antibiotics to treat endocarditis, an infection of the heart’s inner lining.
Effectiveness of Amikacin in Treating Various Infections
Amikacin’s effectiveness in treating infections depends on the specific bacteria causing the infection and the patient’s overall health. It is generally considered a good choice for treating infections caused by multidrug-resistant bacteria, which have become resistant to other antibiotics.
Example: Amikacin is often used to treat infections caused by Pseudomonas aeruginosa, a common cause of hospital-acquired infections that is often resistant to other antibiotics.
Use of Amikacin in Specific Patient Populations
Amikacin is used to treat infections in various patient populations, including children, pregnant women, and those with specific medical conditions. However, its use in these groups requires careful consideration due to potential side effects and risks.
Use in Children
Amikacin is used to treat serious infections in children when other antibiotics are ineffective or not tolerated. However, the dosage and duration of treatment are adjusted based on the child’s age, weight, and kidney function.
Example: Amikacin is often used to treat severe infections in children with cystic fibrosis, a genetic disorder that affects the lungs and other organs.
Use in Pregnant Women
Amikacin should be used during pregnancy only when the potential benefits outweigh the risks to the fetus. It can cross the placenta and may cause potential harm to the developing fetus.
Example: Amikacin may be used during pregnancy to treat serious infections when other antibiotics are ineffective or not tolerated. However, the risks and benefits should be carefully weighed before starting treatment.
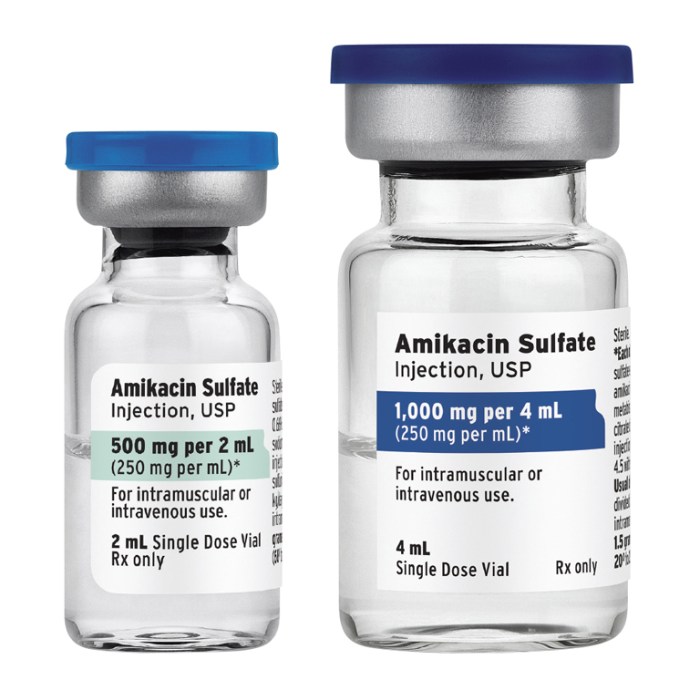
Dosage and Administration of Amikacin
Amikacin is administered intravenously or intramuscularly. The dosage and frequency of administration depend on the severity of the infection, the patient’s renal function, and other factors.
Intravenous Administration
Amikacin is typically administered intravenously over a period of 30 to 60 minutes. This ensures that the drug is delivered into the bloodstream gradually, minimizing the risk of side effects.
Intramuscular Administration, Amikacin
Intramuscular administration is another option for amikacin administration, but it is less common than intravenous administration. This route of administration is suitable for patients who are unable to receive intravenous fluids. The drug is typically injected into a large muscle, such as the gluteus maximus or the deltoid.
Dosage Regimen
The dosage regimen for amikacin varies depending on the severity of the infection, the patient’s renal function, and other factors. A typical dosage regimen for an adult patient with a serious infection is 15 mg/kg of body weight per day, divided into two or three doses. The dosage should be adjusted based on the patient’s renal function, as amikacin is eliminated primarily by the kidneys.
Monitoring Amikacin Levels
Monitoring amikacin levels is crucial to optimize therapy and minimize the risk of toxicity. Serum amikacin levels should be monitored regularly, typically 2 to 4 hours after each dose. This helps ensure that the drug concentration in the bloodstream is within the therapeutic range.
The therapeutic range for amikacin is generally between 5 and 25 mcg/mL.
If the amikacin level is too high, the dosage may need to be reduced or the frequency of administration may need to be adjusted. If the amikacin level is too low, the dosage may need to be increased.
Factors Affecting Amikacin Dosage
Several factors can affect the dosage of amikacin, including:
- Severity of the infection
- Patient’s renal function
- Patient’s age
- Patient’s weight
- Presence of other medical conditions
Monitoring for Adverse Effects
Amikacin can cause various side effects, including:
- Nephrotoxicity
- Ototoxicity
- Hypersensitivity reactions
It is essential to monitor patients for these adverse effects, especially those with pre-existing renal or auditory impairment.
Drug Interactions with Amikacin
Amikacin, like many medications, can interact with other drugs, potentially affecting its effectiveness or increasing the risk of adverse effects. Understanding these interactions is crucial for safe and effective treatment.
Potential Interactions
Amikacin’s interactions can be broadly categorized into two types:
- Pharmacokinetic interactions: These involve changes in the absorption, distribution, metabolism, or elimination of amikacin, leading to altered drug levels in the body.
- Pharmacodynamic interactions: These occur when amikacin’s effects are modified by other drugs, leading to enhanced or diminished therapeutic responses or increased side effects.
Pharmacokinetic Interactions
- Renal Function Impairment: Amikacin is primarily eliminated by the kidneys. Medications that impair renal function, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and aminoglycosides, can increase amikacin levels, potentially leading to toxicity.
- Example: Concurrent use of amikacin with ibuprofen or gentamicin may necessitate dosage adjustments to prevent amikacin accumulation.
- Loop Diuretics: Loop diuretics, such as furosemide and bumetanide, can decrease amikacin levels by increasing renal excretion.
- Example: If a patient is receiving furosemide for heart failure and amikacin for a bacterial infection, the amikacin dosage might need to be increased to maintain therapeutic levels.
- Probenecid: Probenecid, a medication used for gout, can inhibit amikacin excretion, increasing its blood levels.
- Example: A patient taking both probenecid and amikacin might require lower doses of amikacin to avoid toxicity.
Pharmacodynamic Interactions
- Neuromuscular Blocking Agents: Amikacin, like other aminoglycosides, can potentiate the effects of neuromuscular blocking agents, such as succinylcholine and vecuronium, leading to prolonged muscle paralysis.
- Example: During surgery, the use of amikacin may necessitate adjustments in the dosage of neuromuscular blocking agents to avoid prolonged paralysis.
- Ototoxic Drugs: Amikacin’s ototoxicity (damage to the auditory system) can be exacerbated by other ototoxic drugs, such as loop diuretics, vancomycin, and cisplatin.
- Example: Combining amikacin with furosemide for extended periods may increase the risk of hearing loss.
- Nephrotoxic Drugs: Amikacin’s nephrotoxicity (damage to the kidneys) can be amplified by other nephrotoxic drugs, such as NSAIDs, aminoglycosides, and amphotericin B.
- Example: Simultaneous use of amikacin and gentamicin might increase the risk of kidney damage.
Management of Drug Interactions
- Monitoring: Close monitoring of renal function, hearing, and other potential side effects is crucial when amikacin is used in combination with other drugs.
- Example: Regular serum creatinine levels and audiograms can help assess kidney and hearing function.
- Dosage Adjustments: Dose adjustments may be necessary to minimize the risk of interactions and maintain therapeutic efficacy.
- Example: If amikacin is co-administered with a nephrotoxic drug, the dosage may need to be reduced.
- Alternative Medications: When possible, alternative medications with fewer interaction risks may be considered.
- Example: If a patient is allergic to penicillin and needs an antibiotic, amikacin might be a suitable alternative. However, if they are also receiving a nephrotoxic drug, a different antibiotic might be preferred.
Resistance to Amikacin
Amikacin, like other aminoglycosides, faces the challenge of bacterial resistance, which significantly limits its effectiveness in treating infections. Understanding the mechanisms behind this resistance is crucial for optimizing amikacin therapy and combating its decline in clinical utility.
Mechanisms of Amikacin Resistance
Amikacin resistance develops through various mechanisms, primarily involving alterations in the bacterial target site or inactivation of the drug by enzymatic modification.
- Mutations in the 16S rRNA gene: This is a common mechanism where mutations occur in the ribosomal RNA (rRNA) gene, specifically in the 16S rRNA, which is the target site for amikacin binding. These mutations disrupt the interaction between amikacin and the ribosome, reducing its effectiveness in inhibiting protein synthesis.
- Production of aminoglycoside-modifying enzymes (AMEs): Bacteria can produce enzymes that chemically modify amikacin, rendering it inactive. These AMEs are classified into three main groups:
- N-acetyltransferases (AACs): These enzymes add an acetyl group to the amino group of amikacin, reducing its affinity for the ribosome.
- O-phosphotransferases (APHs): These enzymes attach a phosphate group to the hydroxyl group of amikacin, leading to its inactivation.
- O-adenyltransferases (ANTs): These enzymes add an adenyl group to the hydroxyl group of amikacin, rendering it inactive.
- Decreased permeability of the bacterial cell wall: Some bacteria develop resistance by reducing the permeability of their cell wall, making it difficult for amikacin to enter the cell. This can occur through mutations in porin proteins, which are responsible for transporting molecules across the outer membrane.
Prevalence of Amikacin Resistance
Amikacin resistance varies widely among different bacterial species, with some exhibiting higher resistance rates than others.
- Pseudomonas aeruginosa: This bacterium is a common cause of nosocomial infections and often exhibits resistance to amikacin. Resistance rates can vary significantly depending on the geographical location and healthcare setting.
- Acinetobacter baumannii: This bacterium is another significant cause of hospital-acquired infections, and resistance to amikacin is increasingly prevalent.
- Enterobacteriaceae: This family of bacteria, including *Escherichia coli* and *Klebsiella pneumoniae*, can also develop resistance to amikacin. However, resistance rates are generally lower compared to *Pseudomonas aeruginosa* and *Acinetobacter baumannii*.
Impact of Resistance on Amikacin’s Clinical Utility
The emergence of amikacin resistance poses a significant challenge to its clinical utility, limiting its effectiveness in treating infections caused by resistant bacteria.
- Increased treatment failure rates: Infections caused by amikacin-resistant bacteria are more likely to fail treatment, requiring alternative therapies or prolonged hospitalization.
- Limited therapeutic options: The emergence of resistance reduces the number of effective antibiotic options available for treating serious infections, especially in cases where other antibiotics have also failed.
- Increased healthcare costs: Treatment failures due to resistance can lead to prolonged hospital stays, additional diagnostic tests, and the use of more expensive antibiotics, increasing healthcare costs.
- Potential for outbreaks: The spread of amikacin-resistant bacteria can lead to outbreaks in healthcare settings, posing a significant risk to vulnerable patients.
Amikacin in Special Populations
Amikacin’s use in specific patient groups requires careful consideration due to their unique physiological characteristics and potential drug interactions. This section focuses on the administration of amikacin in patients with renal impairment, pediatric patients, and pregnant women.
Amikacin in Patients with Renal Impairment
Renal impairment significantly affects amikacin’s pharmacokinetics, primarily due to its elimination via the kidneys. Therefore, dose adjustments are crucial to prevent amikacin accumulation and potential toxicity.
- Dose Reduction: In patients with reduced renal function, the standard amikacin dose should be reduced to prevent drug accumulation. The recommended dose adjustment is based on the patient’s creatinine clearance (CrCl) value.
- Extended Dosing Intervals: For patients with impaired renal function, extending the dosing interval is often necessary to compensate for the slower drug elimination. This helps maintain therapeutic drug levels while minimizing the risk of toxicity.
- Monitoring: Regular monitoring of serum amikacin levels is crucial in patients with renal impairment. This allows for timely dose adjustments and ensures therapeutic drug levels are maintained while minimizing the risk of toxicity.
Amikacin in Pediatric Patients
The use of amikacin in children requires careful consideration due to their developing organs and potential for adverse effects.
- Dosage Adjustments: Pediatric dosing of amikacin is typically based on body weight and age. Lower doses are generally recommended for children compared to adults.
- Monitoring: Close monitoring of serum amikacin levels is crucial in pediatric patients. This allows for timely dose adjustments and ensures therapeutic drug levels are maintained while minimizing the risk of toxicity.
- Ototoxicity: Children are more susceptible to amikacin-induced ototoxicity than adults. Therefore, careful monitoring of hearing function is essential, particularly with prolonged treatment.
Amikacin in Pregnant Women
The safety and efficacy of amikacin in pregnant women require careful consideration due to the potential for adverse effects on the fetus.
- Limited Data: There are limited data available on the use of amikacin during pregnancy.
- Risk-Benefit Assessment: The decision to use amikacin in pregnant women should be made after a thorough risk-benefit assessment, considering the severity of the infection and the potential risks to the fetus.
- Monitoring: Close monitoring of fetal development is recommended during amikacin treatment in pregnancy.
Future Directions for Amikacin Research
Amikacin, a aminoglycoside antibiotic, has been a mainstay in the treatment of serious bacterial infections for decades. However, the emergence of drug-resistant bacteria and the limitations of current amikacin formulations present significant challenges for its continued effectiveness. Research efforts are ongoing to address these challenges and optimize the therapeutic potential of amikacin.
Development of Novel Amikacin-Based Therapies
The development of novel amikacin-based therapies aims to overcome the limitations of current formulations and enhance the efficacy and safety of amikacin treatment. These efforts focus on improving drug delivery, reducing toxicity, and expanding the spectrum of activity against resistant bacteria.
- Amikacin Prodrugs: Prodrugs are inactive forms of drugs that are converted into active metabolites in the body. Amikacin prodrugs are being developed to improve drug delivery to target tissues and enhance its efficacy. For example, amikacin prodrugs that are specifically targeted to the lungs could be beneficial for treating pulmonary infections.
- Amikacin Conjugates: Conjugation of amikacin with other molecules can improve its pharmacokinetic properties, such as its half-life and distribution. Amikacin conjugates are being explored to enhance drug stability, reduce toxicity, and improve penetration into tissues.
- Amikacin Nanoparticles: Nanoparticles can encapsulate amikacin and protect it from degradation, allowing for sustained release and improved bioavailability. Nanoparticles can also be designed to target specific tissues or cells, enhancing drug delivery and reducing off-target effects.
Amikacin

Amikacin is a potent aminoglycoside antibiotic used to treat serious bacterial infections. It is a valuable therapeutic option, particularly for infections caused by gram-negative bacteria, but its use is accompanied by potential side effects and the emergence of resistance. This comprehensive review will delve into the key aspects of amikacin, including its pharmacokinetic properties, clinical applications, dosage considerations, and potential risks.
Pharmacokinetics of Amikacin
Amikacin is administered intravenously or intramuscularly. It is rapidly distributed throughout the body, achieving therapeutic concentrations in various tissues, including the lungs, kidneys, and bone. However, it does not effectively penetrate the blood-brain barrier. The elimination of amikacin primarily occurs through renal excretion, making it crucial to adjust dosage in patients with impaired kidney function.
Clinical Uses of Amikacin
Amikacin is indicated for the treatment of severe infections caused by susceptible bacteria, particularly gram-negative organisms. It is commonly used for infections such as:
- Lower respiratory tract infections (e.g., pneumonia)
- Urinary tract infections
- Skin and soft tissue infections
- Septicemia
- Endocarditis
Amikacin is often used in combination with other antibiotics, particularly for polymicrobial infections or when resistance to other drugs is a concern.
Dosage and Administration of Amikacin
The dosage of amikacin is determined based on the severity of the infection, the patient’s weight, and renal function. The usual adult dosage is 15 mg/kg per day, administered in divided doses every 8 to 12 hours. However, this dosage may need to be adjusted based on individual factors.
Drug Interactions with Amikacin
Amikacin can interact with other medications, potentially leading to adverse effects. Some notable interactions include:
- Loop diuretics: These medications can increase the risk of amikacin-induced nephrotoxicity.
- Neuromuscular blocking agents: Amikacin can enhance the effects of these agents, leading to prolonged muscle paralysis.
- Other aminoglycosides: Concurrent use with other aminoglycosides increases the risk of nephrotoxicity and ototoxicity.
Resistance to Amikacin
Like other aminoglycosides, amikacin resistance can develop due to various mechanisms, including:
- Enzymatic inactivation of the drug by bacterial enzymes.
- Mutations in ribosomal proteins that decrease the drug’s binding affinity.
- Alterations in bacterial membrane permeability that reduce drug entry.
The emergence of resistance to amikacin is a significant concern, and appropriate antimicrobial stewardship practices are essential to minimize its development.
Amikacin in Special Populations
Amikacin use in specific patient populations requires careful consideration due to potential risks and limitations.
Pregnancy and Lactation
Amikacin should be used during pregnancy only if the potential benefits outweigh the risks. It is known to cross the placenta and may have adverse effects on the fetus.
Pediatric Patients
Amikacin dosage in children should be carefully adjusted based on weight and renal function. It is crucial to monitor for potential side effects, particularly nephrotoxicity and ototoxicity.
Elderly Patients
Older adults are more susceptible to amikacin-induced nephrotoxicity and ototoxicity. Close monitoring of renal function and audiometric testing is essential.
Future Directions for Amikacin Research
Ongoing research focuses on:
- Developing novel aminoglycosides with improved pharmacokinetic profiles and reduced toxicity.
- Investigating strategies to overcome amikacin resistance, such as combination therapy or drug delivery systems.
- Exploring the potential of amikacin in combination with other antibiotics to enhance therapeutic efficacy.
Amikacin: A Comprehensive Review
Amikacin is a potent aminoglycoside antibiotic that remains a valuable therapeutic option for serious bacterial infections. Its effectiveness against gram-negative bacteria, particularly in combination with other antibiotics, makes it an essential component of antimicrobial therapy. However, its use is associated with potential side effects, including nephrotoxicity and ototoxicity, and the emergence of resistance. Therefore, judicious use, appropriate dosage adjustments, and careful monitoring are crucial to optimize therapeutic benefits while minimizing risks.
| Characteristic | Description |
|---|---|
| Mechanism of action | Inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit. |
| Spectrum of activity | Effective against gram-negative bacteria, including Pseudomonas aeruginosa, Escherichia coli, and Klebsiella pneumoniae. |
| Pharmacokinetic properties | Rapidly distributed throughout the body, eliminated primarily through renal excretion. |
| Clinical uses | Severe infections caused by susceptible bacteria, particularly gram-negative organisms. |
| Dosage and administration | Intravenous or intramuscular injection, dosage adjusted based on patient factors. |
| Adverse effects | Nephrotoxicity, ototoxicity, hypersensitivity reactions. |
| Drug interactions | Loop diuretics, neuromuscular blocking agents, other aminoglycosides. |
| Resistance | Can develop due to enzymatic inactivation, ribosomal mutations, or altered membrane permeability. |
| Special populations | Requires careful consideration in pregnant women, children, and elderly patients. |
Amikacin remains a crucial antibiotic in the medical arsenal, offering a powerful line of defense against a variety of infections. Understanding its unique characteristics, appropriate dosage, and potential risks is essential for maximizing its therapeutic benefit and minimizing adverse outcomes. Continued research into amikacin’s mechanisms of action and the development of novel strategies to combat resistance are vital for ensuring its continued relevance in the fight against bacterial infections.
Amikacin is an antibiotic used to treat serious bacterial infections. It’s important to be aware of potential side effects, as with any medication. While amikacin is typically safe, it’s crucial to understand the potential risks associated with its use. For instance, paxil side effects can include nausea, dizziness, and drowsiness, highlighting the importance of monitoring for potential side effects with any medication, including amikacin.