Beta blockers, a class of medications that effectively block the effects of adrenaline and noradrenaline on the heart, have revolutionized the treatment of various cardiovascular conditions. They work by slowing down the heart rate, lowering blood pressure, and reducing the force of heart contractions. Beta blockers have a long and rich history, with their discovery and development marking a significant milestone in the field of medicine.
Since their introduction, beta blockers have become an indispensable tool in the management of a wide range of conditions, including hypertension, angina, heart failure, and even migraine headaches. Their effectiveness in treating these conditions has led to improved quality of life and increased life expectancy for countless individuals.
What are Beta Blockers?
Beta blockers are a class of medications that are primarily used to treat high blood pressure, heart rhythm problems, and other cardiovascular conditions. They work by blocking the effects of adrenaline (epinephrine) and noradrenaline (norepinephrine), hormones that stimulate the heart and blood vessels.
Mechanism of Action
Beta blockers work by blocking the beta receptors in the heart and blood vessels. These receptors are responsible for mediating the effects of adrenaline and noradrenaline. When these receptors are blocked, the heart beats slower and with less force, and the blood vessels relax, which lowers blood pressure.
Beta blockers work by blocking the beta receptors in the heart and blood vessels, which are responsible for mediating the effects of adrenaline and noradrenaline.
Types of Beta Blockers
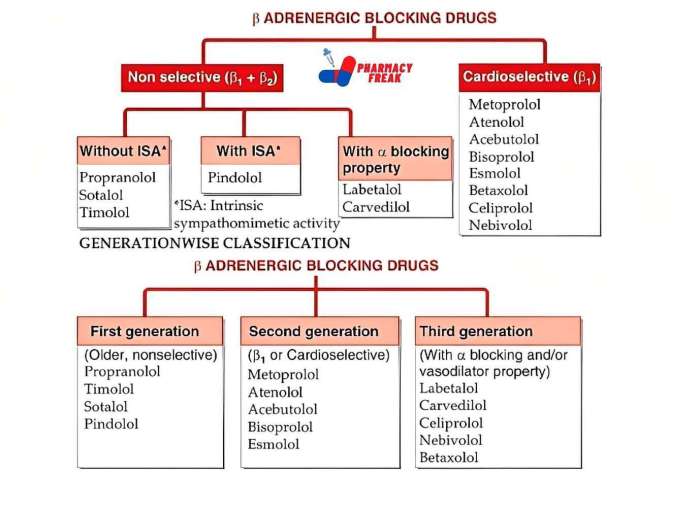
Beta blockers are classified into two main groups:
- Non-selective beta blockers block both beta-1 and beta-2 receptors. These are typically used to treat high blood pressure, heart rhythm problems, and migraine headaches. Examples include propranolol, nadolol, and timolol.
- Selective beta blockers block only beta-1 receptors, which are primarily located in the heart. These are often preferred for treating heart conditions, such as angina and heart failure. Examples include atenolol, metoprolol, and bisoprolol.
Uses of Beta Blockers
Beta blockers are used to treat a wide range of conditions, including:
- High blood pressure: Beta blockers help to lower blood pressure by reducing the heart rate and relaxing the blood vessels.
- Heart rhythm problems: Beta blockers can help to control irregular heart rhythms, such as atrial fibrillation and ventricular tachycardia.
- Angina: Beta blockers can reduce the frequency and severity of angina attacks by reducing the heart’s workload.
- Heart failure: Beta blockers can improve the heart’s pumping ability and reduce the risk of sudden death in patients with heart failure.
- Migraine headaches: Beta blockers can help to prevent migraine headaches by reducing the blood flow to the brain.
- Anxiety disorders: Beta blockers can help to reduce the physical symptoms of anxiety, such as trembling and rapid heartbeat.
History of Beta Blocker Development
The development of beta blockers began in the 1950s with the discovery of propranolol, the first beta blocker to be marketed. This discovery revolutionized the treatment of cardiovascular diseases and had a significant impact on medicine. Since then, many other beta blockers have been developed, with each having its own unique properties and applications.
The discovery of propranolol in the 1950s revolutionized the treatment of cardiovascular diseases and had a significant impact on medicine.
Therapeutic Uses of Beta Blockers
Beta blockers are a class of medications that are widely used to treat a variety of cardiovascular conditions. They work by blocking the effects of adrenaline (epinephrine) and noradrenaline (norepinephrine) on the heart and blood vessels. This results in a decrease in heart rate, blood pressure, and the force of heart contractions.
Beta blockers are effective in treating a range of cardiovascular conditions, including hypertension, angina, and heart failure. They are also used to prevent secondary cardiovascular events in individuals who have already experienced a heart attack or stroke.
Hypertension
Beta blockers are often used as first-line therapy for hypertension, especially in individuals with high heart rate or a history of coronary artery disease. They can effectively lower blood pressure by reducing the heart rate and decreasing the force of heart contractions. Some commonly used beta blockers for hypertension include atenolol, metoprolol, and bisoprolol.
Angina
Beta blockers are a mainstay in the treatment of angina, a condition characterized by chest pain caused by reduced blood flow to the heart muscle. They work by reducing the heart’s oxygen demand, thereby reducing the frequency and severity of angina episodes. Beta blockers are also used to prevent future heart attacks in individuals with a history of angina. Examples of beta blockers commonly used for angina include propranolol, metoprolol, and carvedilol.
Heart Failure
Beta blockers have a significant role in the management of heart failure, a condition where the heart is unable to pump blood effectively. They can improve heart function and reduce the risk of death in patients with heart failure. Beta blockers, such as carvedilol and metoprolol succinate, work by reducing the heart rate and improving the efficiency of the heart’s pumping action.
Prevention of Secondary Cardiovascular Events
Beta blockers play a crucial role in preventing secondary cardiovascular events, such as heart attacks and strokes, in individuals who have already experienced these events. They help to reduce the risk of these events by lowering blood pressure, reducing heart rate, and improving the overall function of the heart. Beta blockers are often recommended for long-term use in individuals with a history of cardiovascular events to prevent future complications.
Pharmacokinetics and Metabolism of Beta Blockers

Beta blockers undergo various processes within the body, including absorption, distribution, metabolism, and elimination. These processes collectively determine the concentration of the drug in the bloodstream and its duration of action. Understanding the pharmacokinetic profile of beta blockers is crucial for optimizing their therapeutic effects and minimizing potential adverse events.
Absorption
Beta blockers are typically administered orally, although some are available intravenously. Oral absorption is generally good for most beta blockers, but it can be influenced by factors such as food intake, gastrointestinal motility, and the specific formulation.
For example, propranolol is absorbed more rapidly when taken on an empty stomach, while metoprolol is less affected by food. The rate of absorption can be affected by factors like food intake and the specific formulation of the drug.
Distribution
Once absorbed, beta blockers distribute throughout the body, primarily binding to plasma proteins. The extent of protein binding varies among different beta blockers, influencing their distribution and volume of distribution.
For example, atenolol has a high volume of distribution, meaning it distributes widely throughout the body, while propranolol has a lower volume of distribution, suggesting it is more concentrated in the bloodstream.
Metabolism
Most beta blockers undergo extensive metabolism in the liver, primarily through the cytochrome P450 enzyme system. Metabolism converts the parent drug into inactive metabolites, which are then eliminated from the body.
The metabolism of beta blockers can be influenced by factors such as age, liver function, and drug interactions.
Elimination
Beta blockers and their metabolites are primarily eliminated through the kidneys. The elimination half-life, which is the time it takes for the plasma concentration of the drug to decrease by half, varies among different beta blockers.
For example, atenolol has a long half-life of about 6-7 hours, while propranolol has a shorter half-life of about 3-6 hours.
Factors Influencing Pharmacokinetics
Several factors can influence the pharmacokinetic profile of beta blockers, including:
- Age: Older adults may have reduced liver and kidney function, which can affect drug metabolism and elimination. This may lead to higher drug levels and an increased risk of adverse effects.
- Liver function: Patients with impaired liver function may have slower drug metabolism, resulting in higher drug levels and a prolonged duration of action.
- Drug interactions: Concomitant use of other medications, particularly those metabolized by the same enzymes, can alter the pharmacokinetic profile of beta blockers. This can lead to increased or decreased drug levels, potentially affecting efficacy or safety.
Drug Accumulation
Repeated dosing of beta blockers can lead to drug accumulation in the body, especially in patients with impaired liver or kidney function. Accumulation can result in higher drug levels and an increased risk of adverse effects.
It is important to monitor patients receiving beta blockers for signs of drug accumulation, such as increased side effects or altered drug levels. Regular monitoring of blood levels can help to ensure that the drug is at a therapeutic level without causing excessive accumulation.
Adverse Effects and Drug Interactions
Beta blockers, while effective in managing various cardiovascular conditions, can also cause adverse effects and interact with other medications. Understanding these potential issues is crucial for safe and effective treatment.
Common Adverse Effects
Beta blockers can affect various bodily systems, leading to a range of adverse effects.
- Fatigue: Beta blockers can slow down the heart rate and reduce blood pressure, leading to fatigue and weakness. This effect is more common with higher doses and may improve with time.
- Bradycardia: A slowed heart rate (bradycardia) is a common side effect of beta blockers. It can be mild and not cause any symptoms, but in some cases, it can lead to dizziness, lightheadedness, and fainting.
- Bronchospasm: Beta blockers can constrict the airways, leading to bronchospasm, particularly in individuals with asthma or other respiratory conditions. This is a serious side effect and may require immediate medical attention.
- Other Adverse Effects: Other common side effects include cold extremities, nausea, vomiting, diarrhea, and constipation. Less common but potentially serious side effects include heart failure, liver problems, and blood disorders.
Drug Interactions
Beta blockers can interact with various medications, including:
- Cardiovascular Drugs: Beta blockers can interact with other cardiovascular drugs, such as calcium channel blockers, digoxin, and nitrates, potentially leading to increased risk of bradycardia, hypotension, and heart failure.
- Antidepressants: Some antidepressants, particularly monoamine oxidase inhibitors (MAOIs) and selective serotonin reuptake inhibitors (SSRIs), can interact with beta blockers, increasing the risk of side effects like hypotension and bradycardia.
- Antihistamines: Certain antihistamines, such as terfenadine and astemizole, can interact with beta blockers, potentially leading to dangerous heart rhythm problems.
Minimizing Risks and Managing Interactions
To minimize the risk of adverse effects and manage potential interactions, consider the following:
- Start with a low dose: Begin with a low dose of the beta blocker and gradually increase it as tolerated. This approach can help minimize the risk of side effects.
- Monitor for side effects: Regularly monitor for any signs or symptoms of adverse effects and report them to your healthcare provider promptly. Early detection and intervention can prevent complications.
- Inform your doctor about all medications: Provide a complete list of all medications, including over-the-counter drugs and supplements, to your doctor to ensure safe and effective treatment.
- Avoid abrupt discontinuation: Never stop taking beta blockers abruptly without consulting your doctor. Sudden withdrawal can lead to rebound hypertension, angina, and other serious complications.
Beta Blockers and Specific Populations
Beta blockers are widely used to treat a variety of cardiovascular conditions, but their use in certain populations requires careful consideration due to unique physiological and pharmacological factors.
Pregnancy and Lactation
Beta blockers can cross the placenta and may have adverse effects on the fetus. The risk of fetal bradycardia, intrauterine growth restriction, and neonatal hypoglycemia is increased with beta blocker use during pregnancy.
- The use of beta blockers in pregnancy should be avoided unless the potential benefits outweigh the risks.
- If beta blocker therapy is necessary, the lowest effective dose should be used, and close fetal monitoring is essential.
- Some beta blockers, such as atenolol and metoprolol, are considered safer in pregnancy than others, such as propranolol and carvedilol.
Beta blockers are also excreted in breast milk, and some may cause adverse effects in the infant.
- If possible, breastfeeding should be avoided during beta blocker therapy.
- If breastfeeding is necessary, the infant should be closely monitored for signs of bradycardia, hypoglycemia, and respiratory distress.
- The choice of beta blocker and the infant’s age and health status should be considered when making decisions about breastfeeding.
Children
The use of beta blockers in children is generally safe and effective when used appropriately. However, the pharmacokinetics and pharmacodynamics of beta blockers may differ in children compared to adults.
- The dosage of beta blockers should be adjusted based on the child’s age, weight, and clinical condition.
- Close monitoring for adverse effects is essential in children.
- Some beta blockers, such as propranolol and atenolol, are available in formulations specifically designed for children.
Renal and Hepatic Impairment
Beta blockers are metabolized primarily by the liver and excreted by the kidneys. Patients with renal or hepatic impairment may experience increased drug accumulation and an increased risk of adverse effects.
- The dosage of beta blockers should be reduced or the dosing interval should be increased in patients with renal or hepatic impairment.
- Close monitoring for adverse effects is essential in these patients.
- Some beta blockers, such as atenolol and metoprolol, are less affected by renal impairment than others, such as propranolol and carvedilol.
Athletes, Beta blockers
Beta blockers are used to treat a variety of cardiovascular conditions, but they can also have adverse effects on athletic performance.
- Beta blockers can reduce heart rate and contractility, which can impair exercise capacity.
- Beta blockers can also interfere with the body’s response to stress and may increase the risk of fatigue and muscle cramps.
- The use of beta blockers in athletes should be carefully considered and only prescribed if the potential benefits outweigh the risks.
Patients with Diabetes
Beta blockers can mask the symptoms of hypoglycemia, such as tachycardia and sweating.
- Patients with diabetes who are taking beta blockers should be closely monitored for signs of hypoglycemia.
- Patients should be educated about the signs and symptoms of hypoglycemia and how to manage it.
- The use of beta blockers in patients with diabetes should be carefully considered, and the potential benefits should be weighed against the risks.
Beta Blockers and Other Cardiovascular Medications
Beta blockers are a class of medications that are commonly used to treat cardiovascular diseases. They are often used in combination with other cardiovascular medications, such as calcium channel blockers, ACE inhibitors, and diuretics. Understanding the mechanisms of action and clinical uses of these medications, as well as their potential benefits and risks when combined, is crucial for optimizing patient care.
Comparison of Mechanisms of Action and Clinical Uses
This section compares and contrasts the mechanisms of action and clinical uses of beta blockers with other cardiovascular medications.
- Beta Blockers: Beta blockers work by blocking the effects of epinephrine (adrenaline) and norepinephrine on beta receptors in the heart, blood vessels, and other tissues. This results in a decrease in heart rate, blood pressure, and myocardial contractility. Beta blockers are commonly used to treat hypertension, angina, heart failure, and arrhythmias.
- Calcium Channel Blockers: Calcium channel blockers work by blocking the influx of calcium ions into vascular smooth muscle cells, leading to vasodilation and a decrease in blood pressure. They are also used to treat angina and arrhythmias.
- ACE Inhibitors: ACE inhibitors block the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. This results in vasodilation, a decrease in blood pressure, and a reduction in aldosterone secretion. ACE inhibitors are commonly used to treat hypertension, heart failure, and diabetic nephropathy.
- Diuretics: Diuretics increase urine production, leading to a decrease in blood volume and blood pressure. They are commonly used to treat hypertension, heart failure, and edema.
Benefits and Risks of Combining Beta Blockers with Other Cardiovascular Medications
Combining beta blockers with other cardiovascular medications can offer several benefits, including:
- Enhanced therapeutic efficacy: Combining medications can lead to a synergistic effect, resulting in greater blood pressure reduction or improved control of other cardiovascular symptoms.
- Reduced risk of adverse effects: Combining medications can allow for lower doses of each individual drug, potentially reducing the risk of side effects.
However, combining medications also carries potential risks, including:
- Increased risk of adverse effects: Some medications may interact with each other, increasing the risk of side effects.
- Drug interactions: Certain medications can interact with each other, affecting their absorption, metabolism, or excretion.
Examples of Medication Combinations and Their Therapeutic Implications
Here are some examples of specific medication combinations and their therapeutic implications:
- Beta blocker + calcium channel blocker: This combination is often used to treat hypertension and angina. The beta blocker reduces heart rate and contractility, while the calcium channel blocker dilates blood vessels.
- Beta blocker + ACE inhibitor: This combination is often used to treat heart failure. The beta blocker reduces heart rate and contractility, while the ACE inhibitor reduces blood pressure and improves cardiac function.
- Beta blocker + diuretic: This combination is often used to treat hypertension and edema. The beta blocker reduces heart rate and contractility, while the diuretic reduces blood volume and blood pressure.
Patient Education and Counseling
This brochure provides essential information about beta blockers, a type of medication commonly used to treat various heart conditions. Understanding your medication is crucial for managing your health effectively.
Important Information About Beta Blockers
Beta blockers are medications that block the effects of adrenaline (epinephrine) and noradrenaline (norepinephrine) on your heart and blood vessels. These hormones naturally increase your heart rate and blood pressure. By blocking their effects, beta blockers help to:
* Lower your heart rate: This reduces the workload on your heart.
* Lower your blood pressure: This eases the strain on your blood vessels.
* Reduce the risk of heart attacks and strokes: By lowering blood pressure and heart rate, beta blockers can help to prevent these serious events.
Potential Side Effects of Beta Blockers
Like all medications, beta blockers can cause side effects, although not everyone experiences them. Some common side effects include:
* Fatigue: Feeling tired or weak.
* Dizziness: Feeling lightheaded or unsteady.
* Headache: A throbbing or dull pain in your head.
* Cold hands and feet: Reduced blood flow to your extremities.
* Shortness of breath: Difficulty breathing.
* Depression: Feeling sad or hopeless.
* Sexual dysfunction: Difficulty achieving or maintaining an erection.
Safe Use of Beta Blockers
To ensure safe and effective use of beta blockers, it is important to follow these guidelines:
* Take your medication as prescribed: Do not skip doses or take more than the recommended amount.
* Do not stop taking your medication abruptly: Talk to your doctor before making any changes to your medication regimen.
* Inform your doctor about any other medications you are taking: This includes over-the-counter medications, herbal supplements, and vitamins.
* Monitor your blood pressure and heart rate regularly: This will help you and your doctor track the effectiveness of your medication.
* Report any side effects to your doctor: If you experience any unusual or bothersome side effects, contact your doctor immediately.
* Avoid alcohol consumption: Alcohol can interact with beta blockers and increase the risk of side effects.
* Eat a healthy diet and exercise regularly: These lifestyle changes can help to improve your overall health and reduce the risk of heart disease.
Common Questions About Beta Blockers
- What are beta blockers used for? Beta blockers are primarily used to treat high blood pressure, angina (chest pain), irregular heartbeat, and heart failure. They are also sometimes used to prevent migraines and reduce the risk of heart attacks and strokes.
- How do beta blockers work? Beta blockers block the effects of adrenaline and noradrenaline on your heart and blood vessels, which helps to lower your heart rate and blood pressure.
- What are the potential side effects of beta blockers? Some common side effects include fatigue, dizziness, headache, cold hands and feet, shortness of breath, depression, and sexual dysfunction. It is important to note that not everyone experiences these side effects.
- How long do I need to take beta blockers? The duration of treatment with beta blockers varies depending on your individual condition and response to medication. Your doctor will determine the appropriate duration of treatment.
- Can I stop taking beta blockers suddenly? No, it is not recommended to stop taking beta blockers suddenly. Doing so can lead to a rebound effect, which can worsen your condition. You should always talk to your doctor before making any changes to your medication regimen.
- What if I miss a dose of beta blockers? If you miss a dose of beta blockers, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular schedule. Do not double the dose to make up for a missed dose.
- Can I drink alcohol while taking beta blockers? It is generally advisable to avoid alcohol consumption while taking beta blockers, as alcohol can interact with the medication and increase the risk of side effects.
- Can I take beta blockers with other medications? It is important to inform your doctor about all medications you are taking, including over-the-counter medications, herbal supplements, and vitamins. Beta blockers can interact with certain medications, so it is crucial to avoid potential drug interactions.
- What are the long-term effects of beta blockers? Beta blockers are generally safe for long-term use. However, it is important to monitor for any potential side effects and to discuss any concerns with your doctor.
Counseling Session
During a counseling session, your doctor or pharmacist will discuss your medication in detail, including:
* Your specific condition and why beta blockers are prescribed: This will help you understand the rationale behind your treatment.
* How to take your medication correctly: This includes the dosage, frequency, and timing of your doses.
* Potential side effects and how to manage them: You will learn about the possible side effects and how to minimize their impact.
* Safe use of beta blockers: This includes avoiding alcohol consumption, informing your doctor about other medications you are taking, and monitoring your blood pressure and heart rate regularly.
* What to do if you miss a dose: You will learn how to handle missed doses without compromising your treatment.
* How to contact your doctor or pharmacist if you have any questions or concerns: It is important to stay in touch with your healthcare provider to ensure safe and effective medication management.
This counseling session is designed to empower you to manage your medication effectively and make informed decisions about your health.
Research and Future Directions: Beta Blockers
Beta blockers have been a mainstay in cardiovascular medicine for decades, but ongoing research continues to reveal new applications and refine our understanding of their efficacy and safety. Research efforts are exploring novel uses for existing beta blockers, developing new beta blockers with enhanced properties, and investigating the underlying mechanisms of action.
New Therapeutic Applications
Ongoing research is exploring the potential of beta blockers in a wider range of therapeutic areas beyond cardiovascular disease. For example, studies have suggested that beta blockers might be beneficial in conditions like:
- Migraine headaches: Beta blockers are known to reduce the frequency and severity of migraine headaches, possibly by reducing vascular dilation and neurotransmitter release.
- Anxiety disorders: Some beta blockers, such as propranolol, have been shown to reduce anxiety symptoms by blocking the effects of adrenaline and noradrenaline on the nervous system.
- Essential tremor: Beta blockers can help control tremors by blocking the effects of adrenaline on the nervous system, which can contribute to tremor.
- Hyperthyroidism: Beta blockers can be used to control the symptoms of hyperthyroidism by blocking the effects of thyroid hormones on the heart and other organs.
Improving Understanding of Beta Blocker Efficacy and Safety
While beta blockers are generally safe and effective, there are still areas where further research is needed to improve our understanding of their efficacy and safety.
- Long-term safety: Long-term studies are needed to evaluate the long-term safety of beta blockers, particularly in specific populations such as children and pregnant women.
- Individualized dosing: Research is ongoing to develop personalized dosing strategies for beta blockers, taking into account factors such as age, genetics, and co-morbidities.
- Interactions with other medications: Further research is needed to understand the potential interactions between beta blockers and other medications, especially those used for other cardiovascular conditions.
- Effects on specific populations: More research is needed to understand the effects of beta blockers on specific populations, such as individuals with diabetes, asthma, or kidney disease.
Developing Novel Beta Blockers
Researchers are actively developing novel beta blockers with improved properties, such as:
- Enhanced selectivity: Novel beta blockers are being developed with greater selectivity for beta-1 receptors, which are predominantly found in the heart, minimizing the potential for side effects on other organs.
- Improved pharmacokinetic properties: Researchers are exploring new beta blockers with longer half-lives, allowing for less frequent dosing and potentially improving patient adherence.
- Reduced adverse effects: New beta blockers are being developed with fewer adverse effects, such as fatigue, dizziness, and sexual dysfunction.
- New delivery systems: Research is investigating novel delivery systems for beta blockers, such as transdermal patches and sustained-release formulations, to improve patient convenience and compliance.
Beta Blockers in the Treatment of Anxiety

Beta blockers are a class of medications primarily used to treat cardiovascular conditions, such as high blood pressure and heart disease. However, they have also been found to be effective in managing certain symptoms of anxiety disorders. Beta blockers work by blocking the effects of adrenaline, a hormone that is released in response to stress and can cause physical symptoms such as rapid heart rate, trembling, and sweating.
Beta Blockers and the Management of Physical Anxiety Symptoms
Beta blockers are particularly helpful in managing the physical symptoms of anxiety, such as:
* Rapid heart rate (tachycardia): Beta blockers slow down the heart rate by blocking the effects of adrenaline on the heart.
* Tremors: Beta blockers can reduce tremors by blocking the effects of adrenaline on the muscles.
* Sweating (hyperhidrosis): Beta blockers can decrease sweating by blocking the effects of adrenaline on the sweat glands.
* Flushing: Beta blockers can reduce flushing by blocking the effects of adrenaline on the blood vessels.
* Shortness of breath: Beta blockers can improve breathing by relaxing the airways and reducing the heart rate.
While beta blockers are effective in managing physical anxiety symptoms, they do not address the underlying causes of anxiety.
Comparison of Beta Blockers with Other Anxiety Medications
Beta blockers are not typically considered first-line treatment for anxiety disorders. Other medications, such as selective serotonin reuptake inhibitors (SSRIs) and benzodiazepines, are more commonly used for anxiety. However, beta blockers can be a useful adjunct therapy for patients who experience significant physical anxiety symptoms.
Beta blockers differ from other anxiety medications in several ways:
* Mechanism of action: Beta blockers work by blocking the effects of adrenaline, while SSRIs and benzodiazepines work on different neurotransmitter systems in the brain.
* Speed of action: Beta blockers work quickly, within minutes, to reduce physical anxiety symptoms, while SSRIs and benzodiazepines take several weeks to reach their full effect.
* Duration of action: Beta blockers have a shorter duration of action than SSRIs and benzodiazepines, lasting only a few hours.
* Side effects: Beta blockers can cause side effects such as fatigue, dizziness, and low blood pressure. SSRIs and benzodiazepines can also cause side effects, but they are different from those of beta blockers.
Examples of Beta Blockers Commonly Used for Anxiety
Some commonly used beta blockers for anxiety include:
* Propranolol (Inderal): Propranolol is a non-selective beta blocker that is available in immediate-release and extended-release formulations. The typical dosage for anxiety is 10-40 mg, taken 30-60 minutes before an anxiety-provoking event.
* Atenolol (Tenormin): Atenolol is a selective beta blocker that is typically used for high blood pressure. However, it can also be used for anxiety in doses of 25-100 mg, taken once daily.
* Metoprolol (Lopressor, Toprol XL): Metoprolol is another selective beta blocker that is available in immediate-release and extended-release formulations. The typical dosage for anxiety is 25-100 mg, taken twice daily.
It is important to note that beta blockers should only be used under the supervision of a healthcare professional. The dosage and type of beta blocker will vary depending on the individual’s needs and medical history.
Beta Blockers in Migraine Prophylaxis
Beta blockers have been used for migraine prevention for several decades, and their efficacy in reducing migraine frequency and severity has been well-established. These medications work by blocking the effects of certain neurotransmitters and hormones that are involved in migraine attacks.
Mechanism of Action
Beta blockers are thought to prevent migraines by reducing the changes in blood vessel diameter that occur during a migraine attack. During a migraine, blood vessels in the brain constrict, followed by a period of dilation. This vascular fluctuation is thought to trigger the pain and other symptoms of migraine. Beta blockers, by blocking the action of norepinephrine and other vasoconstrictors, help to prevent this vasoconstriction and subsequent dilation, thereby reducing the likelihood of a migraine attack.
Effectiveness of Beta Blockers
Beta blockers are generally considered to be effective for migraine prophylaxis, although their effectiveness varies among individuals. Studies have shown that beta blockers can reduce the frequency of migraine attacks by 50% or more in some patients. However, it’s important to note that beta blockers are not a cure for migraines and they may not be effective for all individuals.
Examples of Beta Blockers Used for Migraine Prevention
Several beta blockers are commonly used for migraine prevention, including:
- Propranolol (Inderal)
- Metoprolol (Lopressor, Toprol XL)
- Atenolol (Tenormin)
- Timolol (Blocadren)
Dosage Regimens
The dosage of beta blockers for migraine prevention varies depending on the specific medication and the individual patient’s needs. Dosage adjustments may be necessary to achieve optimal results.
For example, propranolol is typically started at a low dose of 40-80 mg per day, and the dose can be increased gradually as needed, up to a maximum of 320 mg per day.
Beta blockers have emerged as powerful medications that have transformed the landscape of cardiovascular medicine. Their versatility, effectiveness, and ongoing research continue to make them an integral part of treating and managing various health conditions. Understanding their mechanism of action, therapeutic uses, and potential side effects is crucial for healthcare professionals and patients alike. As research continues to explore new applications for beta blockers, their impact on medicine is likely to grow even further.
Beta blockers are commonly used to treat high blood pressure and heart conditions. They work by blocking the effects of adrenaline, which can help to slow down the heart rate and lower blood pressure. While beta blockers focus on the heart, managing blood sugar levels is also important, especially for those with diabetes. Regular insulin, like the type found here , plays a crucial role in regulating blood sugar.
It’s important to note that beta blockers can sometimes interfere with the effects of insulin, so close monitoring of blood sugar levels is essential for patients taking both medications.