Keflex, also known as cephalexin, is a widely prescribed antibiotic that belongs to the cephalosporin class. It is a versatile drug used to treat a range of bacterial infections, including skin infections, respiratory infections, and urinary tract infections. Keflex works by inhibiting the synthesis of bacterial cell walls, effectively stopping the growth and multiplication of bacteria.
This comprehensive guide will delve into the multifaceted nature of Keflex, covering its chemical structure, mechanism of action, therapeutic applications, pharmacokinetic profile, adverse effects, and drug interactions. We will also explore its use in specific patient populations, including children, pregnant women, and the elderly, as well as address concerns regarding antibiotic resistance and stewardship.
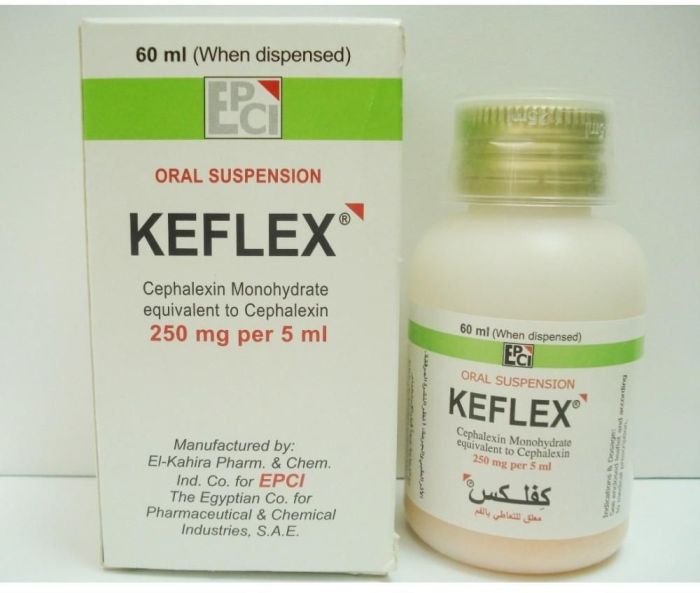
Keflex
Keflex, also known by its generic name cephalexin, is a widely prescribed antibiotic that belongs to the cephalosporin class of drugs. It is commonly used to treat a variety of bacterial infections, including skin infections, respiratory infections, and urinary tract infections.
Chemical Structure and Classification, Keflex
Keflex is a semi-synthetic antibiotic derived from the natural antibiotic cephalosporin C. Its chemical structure is characterized by a beta-lactam ring, which is essential for its antibacterial activity. Cephalexin is classified as a first-generation cephalosporin, meaning it has a broad spectrum of activity against gram-positive bacteria, including *Staphylococcus aureus*, *Streptococcus pyogenes*, and *Streptococcus pneumoniae*. It also exhibits some activity against gram-negative bacteria, such as *Escherichia coli* and *Proteus mirabilis*.
Mechanism of Action
Keflex exerts its antibacterial effect by inhibiting the synthesis of peptidoglycan, a key component of bacterial cell walls. This inhibition prevents bacteria from building and maintaining their cell walls, ultimately leading to cell lysis and death. Specifically, cephalexin binds to and inhibits the activity of bacterial transpeptidases, also known as penicillin-binding proteins (PBPs). These enzymes are crucial for the formation of peptide cross-links in peptidoglycan, which provides structural integrity to the bacterial cell wall. By blocking the activity of these enzymes, Keflex disrupts the synthesis of peptidoglycan, resulting in weakened cell walls and bacterial death.
Forms and Uses
Keflex is available in various forms, including:
- Oral capsules: The most common form, convenient for oral administration. These capsules are typically taken every 6 hours with a full glass of water.
- Oral suspension: This liquid form is particularly useful for children and individuals who have difficulty swallowing capsules.
- Intravenous solution: For severe infections or when oral administration is not possible, Keflex can be administered intravenously.
The choice of formulation depends on the severity of the infection, patient preference, and the ability to swallow medications.
Dosage and Administration
The recommended dosage of Keflex varies depending on the type of infection, patient age, weight, and kidney function. It is crucial to consult with a healthcare professional to determine the appropriate dosage and duration of treatment.
- Adults: The typical dosage for adults is 250-500 mg every 6 hours. For severe infections, the dosage may be increased to 1 gram every 6 hours.
- Children: The dosage for children is based on weight, typically 25-50 mg/kg per day, divided into four doses.
Keflex is usually administered orally, but in cases of severe infections or when oral administration is not possible, it can be given intravenously.
Important Considerations
- Allergic reactions: Like other antibiotics, Keflex can cause allergic reactions in some individuals. Signs of an allergic reaction include rash, itching, swelling, and difficulty breathing. If you experience any of these symptoms, stop taking Keflex immediately and seek medical attention.
- Gastrointestinal side effects: Common side effects of Keflex include nausea, vomiting, diarrhea, and stomach cramps. These side effects are usually mild and often resolve on their own.
- Kidney function: Keflex is primarily excreted by the kidneys. Individuals with impaired kidney function may require dosage adjustments to prevent drug accumulation and potential toxicity.
- Drug interactions: Keflex can interact with certain medications, including those that affect blood clotting, diuretics, and certain types of antibiotics. It is important to inform your healthcare provider about all medications you are taking, including over-the-counter drugs and herbal supplements.
Therapeutic Applications of Keflex
Keflex, also known as cephalexin, is a broad-spectrum antibiotic belonging to the cephalosporin class. It is commonly prescribed for a variety of bacterial infections, exhibiting effectiveness against a wide range of gram-positive and some gram-negative bacteria.
Skin Infections
Keflex is frequently used to treat skin infections caused by susceptible bacteria. It is effective against common skin infections like impetigo, cellulitis, and folliculitis. Keflex is administered orally, making it a convenient option for treating skin infections. It works by interfering with the synthesis of peptidoglycans, essential components of bacterial cell walls, leading to bacterial cell death.
Respiratory Infections
Keflex is also prescribed for respiratory infections, particularly those caused by susceptible strains of Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. It is effective against conditions like otitis media (middle ear infection), sinusitis, and bronchitis. However, Keflex is not typically used for severe pneumonia or other serious respiratory infections.
Urinary Tract Infections
Keflex is often prescribed for uncomplicated urinary tract infections (UTIs), especially those caused by susceptible strains of Escherichia coli. It is administered orally and achieves therapeutic concentrations in the urine, effectively combating bacterial growth in the urinary tract. However, Keflex may not be suitable for complicated UTIs or those involving resistant bacteria.
Comparison with Other Antibiotics
Keflex is often compared to other antibiotics commonly used to treat similar conditions, such as amoxicillin, penicillin, and doxycycline.
- Amoxicillin, another broad-spectrum antibiotic, is often considered a first-line treatment for skin and respiratory infections. It is generally well-tolerated, but Keflex may be preferred in cases of penicillin allergy or when amoxicillin resistance is suspected.
- Penicillin is a narrow-spectrum antibiotic effective against a limited range of bacteria. It is typically used for infections caused by penicillin-susceptible organisms. Keflex offers broader coverage and may be a better option when the causative organism is unknown or when penicillin resistance is suspected.
- Doxycycline, a tetracycline antibiotic, is also effective against a broad range of bacteria. It is commonly used for skin infections, respiratory infections, and UTIs. However, Keflex may be preferred for certain infections, particularly those involving specific bacterial strains or when doxycycline is contraindicated.
Pharmacokinetic Profile of Keflex

Keflex, or cephalexin, is a cephalosporin antibiotic that is widely used to treat bacterial infections. Its pharmacokinetic profile, which encompasses its absorption, distribution, metabolism, and elimination, is crucial for understanding its therapeutic efficacy and potential side effects.
Absorption
Cephalexin is well absorbed from the gastrointestinal tract after oral administration. Its bioavailability, which refers to the fraction of the drug that reaches systemic circulation, is approximately 90%. The rate and extent of absorption may be affected by the presence of food, with lower peak plasma concentrations observed when Keflex is taken with meals.
Distribution
Once absorbed, cephalexin is distributed throughout the body, primarily to the interstitial fluid and tissues. It penetrates well into most body fluids, including the cerebrospinal fluid, but to a lesser extent in the presence of inflammation. Keflex binds to plasma proteins to a moderate extent, with a protein binding of around 15-25%. This binding can influence its distribution and elimination.
Metabolism
Cephalexin undergoes minimal metabolism in the liver. It is primarily eliminated unchanged in the urine.
Elimination
The elimination half-life of cephalexin is approximately 0.5-2 hours in adults with normal renal function. This means that it takes about 0.5-2 hours for the concentration of the drug in the body to decrease by half. Renal excretion is the primary route of elimination, with approximately 90% of the administered dose being excreted unchanged in the urine.
Influence of Age, Renal Function, and Hepatic Function
Several factors can influence the pharmacokinetics of Keflex, including age, renal function, and hepatic function.
Age
The pharmacokinetics of Keflex may be altered in older adults, as their renal function may decline with age. This can lead to increased drug accumulation and a higher risk of adverse effects.
Renal Function
Renal function plays a significant role in the elimination of Keflex. In patients with impaired renal function, the elimination half-life of the drug may be prolonged, leading to increased drug accumulation and a higher risk of adverse effects. Dosage adjustments may be necessary to account for decreased renal clearance.
Hepatic Function
As cephalexin undergoes minimal metabolism in the liver, hepatic function has a limited impact on its pharmacokinetics. However, in patients with severe hepatic impairment, the elimination of the drug may be slightly delayed.
Pharmacokinetic Parameters of Keflex
The table below summarizes the pharmacokinetic parameters of Keflex:
| Parameter | Value |
|---|---|
| Half-life | 0.5-2 hours |
| Bioavailability | ~90% |
| Protein binding | 15-25% |
Adverse Effects and Drug Interactions: Keflex
Keflex, like most medications, can cause adverse effects and interact with other drugs. It is crucial to understand these potential issues to ensure safe and effective treatment.
Common Adverse Effects
Common adverse effects of Keflex are generally mild and usually resolve on their own. These include:
- Diarrhea
- Nausea
- Vomiting
- Abdominal pain
- Rash
- Yeast infections
Serious Adverse Effects
While less common, Keflex can cause serious adverse effects. These require immediate medical attention and include:
- Anaphylaxis: A severe allergic reaction that can be life-threatening. Symptoms include difficulty breathing, swelling of the face and throat, and a rapid heartbeat.
- Hepatitis: Inflammation of the liver, which can cause jaundice (yellowing of the skin and eyes), abdominal pain, and fatigue.
- Pseudomembranous colitis: A serious intestinal infection caused by Clostridium difficile bacteria. Symptoms include severe diarrhea, abdominal cramps, and fever.
- Blood disorders: Keflex can sometimes cause changes in blood cell counts, which can increase the risk of infections or bleeding.
- Kidney problems: Keflex can damage the kidneys, especially in people with pre-existing kidney disease.
Drug Interactions
Keflex can interact with other medications, potentially affecting their effectiveness or increasing the risk of side effects.
Interactions with Other Antibiotics
Keflex should not be used with other antibiotics, such as erythromycin or clindamycin, as this can increase the risk of serious side effects.
Interactions with Anticoagulants
Keflex can increase the risk of bleeding when taken with anticoagulants, such as warfarin. This is because Keflex can affect the way the body breaks down warfarin.
Interactions with Oral Contraceptives
Keflex may reduce the effectiveness of oral contraceptives. This is because Keflex can affect the way the body breaks down estrogen, one of the hormones in oral contraceptives.
Monitoring Patients on Keflex Therapy
Patients on Keflex therapy should be monitored for potential side effects and drug interactions. This includes:
- Monitoring for signs and symptoms of allergic reactions, such as rash, itching, swelling, and difficulty breathing.
- Monitoring for signs and symptoms of liver problems, such as jaundice, abdominal pain, and fatigue.
- Monitoring for signs and symptoms of intestinal problems, such as severe diarrhea, abdominal cramps, and fever.
- Monitoring blood cell counts to check for any abnormalities.
- Monitoring kidney function, especially in people with pre-existing kidney disease.
- Informing patients about the potential for drug interactions and encouraging them to report any new or worsening symptoms.
Keflex and Pregnancy and Lactation
Keflex, a cephalosporin antibiotic, is commonly prescribed for bacterial infections. However, its use during pregnancy and lactation requires careful consideration due to potential risks to the developing fetus and infant. This section will delve into the safety of Keflex use during these crucial periods, examining the potential risks and benefits of therapy.
Safety of Keflex during Pregnancy
The safety of Keflex during pregnancy is a complex issue. While Keflex has been classified as a category B drug by the Food and Drug Administration (FDA), meaning that studies in animals have not shown any harm to the fetus, there is limited human data available. This classification indicates that the potential benefits of Keflex may outweigh the potential risks in certain situations. However, it is essential to weigh the potential risks and benefits carefully before prescribing Keflex to pregnant women.
Potential Risks of Keflex during Pregnancy
There are potential risks associated with Keflex use during pregnancy, although the evidence is not conclusive. Some studies suggest a possible association between Keflex use during pregnancy and an increased risk of certain birth defects, such as cleft palate and neural tube defects. However, these studies are limited and require further investigation.
Potential Benefits of Keflex during Pregnancy
In some cases, the benefits of treating a bacterial infection with Keflex during pregnancy may outweigh the potential risks. For example, if a pregnant woman has a severe infection that could threaten her health or the health of the fetus, Keflex may be the best treatment option.
Alternative Antibiotic Options for Pregnant Women
If Keflex is not considered safe for a pregnant woman, there are several alternative antibiotic options available. These options include:
- Penicillins: Penicillins are generally considered safe for use during pregnancy. Amoxicillin and penicillin V are commonly used options.
- Erythromycin: Erythromycin is another safe alternative for pregnant women. It is often used to treat respiratory infections and skin infections.
- Clindamycin: Clindamycin is a safe alternative for pregnant women, although it is not typically recommended for use in the first trimester.
Safety of Keflex during Lactation
Keflex is excreted in breast milk in small amounts. While these amounts are generally considered safe for infants, it is important to monitor the infant for any potential adverse effects.
Potential Risks of Keflex during Lactation
The potential risks of Keflex use during lactation include:
- Diarrhea: Keflex can cause diarrhea in infants who are breastfed by mothers taking the drug.
- Allergic reactions: Infants may develop allergic reactions to Keflex, such as rash, hives, or swelling.
- Yeast infections: Keflex can disrupt the normal bacterial balance in the gut, increasing the risk of yeast infections in infants.
Alternative Antibiotic Options for Lactating Women
If Keflex is not considered safe for a lactating woman, there are several alternative antibiotic options available. These options include:
- Penicillins: Penicillins are generally considered safe for use during lactation. Amoxicillin and penicillin V are commonly used options.
- Erythromycin: Erythromycin is another safe alternative for lactating women. It is often used to treat respiratory infections and skin infections.
- Clindamycin: Clindamycin is a safe alternative for lactating women, although it is not typically recommended for use in the first trimester.
Keflex Resistance and Antibiotic Stewardship
Keflex resistance is a growing concern in the medical community, as it can significantly impact the effectiveness of this antibiotic. Understanding the mechanisms of resistance and implementing strategies for antibiotic stewardship are crucial to mitigating this issue.
Mechanisms of Bacterial Resistance to Keflex
The development of resistance to Keflex is a complex process that involves various mechanisms, including:
- Inactivation of Keflex by bacterial enzymes: Some bacteria produce enzymes, such as beta-lactamases, that can break down Keflex, rendering it ineffective. This mechanism is prevalent in strains of Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus (MRSA).
- Alteration of the bacterial target site: Keflex works by inhibiting the synthesis of peptidoglycans, essential components of bacterial cell walls. Bacteria can develop mutations in the genes that code for these proteins, preventing Keflex from binding and inhibiting their function.
- Reduced permeability of the bacterial cell wall: Some bacteria can develop mechanisms that decrease the permeability of their cell wall, limiting the entry of Keflex into the cell. This can be achieved through mutations in the genes responsible for cell wall transport.
- Active efflux pumps: Bacteria can express efflux pumps that actively pump Keflex out of the cell, preventing it from reaching its target site.
Implications of Keflex Resistance on Treatment Outcomes
Keflex resistance can significantly impact treatment outcomes, leading to:
- Treatment failure: When bacteria are resistant to Keflex, the antibiotic may not be effective in treating the infection, leading to prolonged illness and potential complications.
- Increased healthcare costs: Treatment failures due to resistance can lead to prolonged hospital stays, the need for more expensive alternative antibiotics, and increased healthcare costs overall.
- Spread of resistant bacteria: Resistant bacteria can spread to other individuals, contributing to the rise of antibiotic-resistant infections within communities and healthcare settings.
Strategies for Promoting Antibiotic Stewardship and Preventing the Emergence of Resistance
Antibiotic stewardship is a multi-faceted approach that aims to optimize antibiotic use, minimize the development of resistance, and improve patient outcomes. Key strategies include:
- Appropriate prescribing: Prescribing Keflex only when clinically indicated and for the appropriate duration can help minimize the selection pressure for resistant bacteria.
- Culture and sensitivity testing: Performing culture and sensitivity tests to identify the causative organism and its susceptibility to antibiotics is essential for selecting the most effective treatment.
- Education and awareness: Educating healthcare professionals and patients about antibiotic resistance and the importance of appropriate antibiotic use is crucial for promoting stewardship.
- Infection control measures: Implementing strict infection control measures, such as hand hygiene and isolation of patients with resistant infections, can help prevent the spread of resistant bacteria.
- Development of new antibiotics: Ongoing research and development of new antibiotics with novel mechanisms of action are essential for combating the threat of antibiotic resistance.
Keflex in Pediatric and Geriatric Populations
Keflex, like other antibiotics, requires special considerations when used in children and elderly individuals due to their unique physiological characteristics and potential for drug interactions. This section will explore the specific considerations for Keflex use in these populations, including dosage adjustments and monitoring recommendations.
Dosage Adjustments in Pediatric Patients
Dosage adjustments are crucial in pediatric patients to ensure safe and effective therapy. Children’s pharmacokinetic profiles differ significantly from adults, with faster metabolism and altered drug distribution. This necessitates careful calculation of Keflex doses based on the child’s weight and age.
- Weight-Based Dosing: Keflex dosage is typically determined by the child’s weight, often expressed in milligrams per kilogram (mg/kg) of body weight. This approach ensures that the drug concentration in the body is appropriate for the child’s size and metabolic rate.
- Age Considerations: While weight-based dosing is the primary factor, age can also influence dosage adjustments. For instance, infants and toddlers may require more frequent dosing compared to older children due to their faster drug metabolism.
- Clinical Monitoring: Regular monitoring of the child’s response to Keflex therapy is essential. This includes evaluating the effectiveness of the antibiotic in treating the infection and monitoring for any adverse effects.
Dosage Adjustments in Geriatric Patients
Elderly individuals often experience age-related physiological changes that can impact drug pharmacokinetics. These changes include decreased renal function, slower metabolism, and altered drug distribution, which can lead to higher drug accumulation and an increased risk of adverse effects.
- Renal Function Assessment: Assessing renal function is crucial in elderly patients, as Keflex is primarily eliminated through the kidneys. A reduced glomerular filtration rate (GFR) can lead to drug accumulation and an increased risk of toxicity.
- Lower Starting Doses: Initial doses of Keflex should be lower in elderly patients compared to younger adults to minimize the risk of adverse effects.
- Dosing Frequency: Dosing frequency may need to be adjusted based on the patient’s renal function. For individuals with impaired renal function, lower doses or less frequent administration may be necessary.
Monitoring Keflex Therapy in Pediatric and Geriatric Patients
Regardless of age, monitoring Keflex therapy is essential to ensure effectiveness and minimize potential risks.
- Clinical Response: Closely monitor the patient’s response to therapy, including fever resolution, improvement in symptoms, and resolution of the underlying infection.
- Adverse Effects: Monitor for potential adverse effects, such as diarrhea, nausea, vomiting, rash, and allergic reactions.
- Laboratory Monitoring: Regular laboratory tests may be necessary to assess renal function, liver function, and complete blood count, particularly in patients with underlying medical conditions or those receiving prolonged therapy.
Keflex and Allergic Reactions
Keflex, like other penicillin-class antibiotics, can trigger allergic reactions in some individuals. These reactions can range from mild to severe and, in rare cases, can be life-threatening. Understanding the signs, symptoms, and management of Keflex-related allergies is crucial for patient safety.
Signs and Symptoms of Allergic Reactions
Allergic reactions to Keflex can manifest in various ways, depending on the severity of the reaction. Common symptoms include:
- Skin rash: This is often the first sign of a Keflex allergy. It can appear as a red, itchy rash, hives, or even blistering.
- Itching: Generalized itching, especially on the skin, can be a symptom of a mild allergic reaction.
- Swelling: Swelling of the face, lips, tongue, or throat can be a sign of a more severe allergic reaction. This swelling can interfere with breathing and requires immediate medical attention.
- Wheezing or difficulty breathing: These symptoms may indicate an allergic reaction involving the airways, known as bronchospasm.
- Anaphylaxis: Anaphylaxis is a life-threatening allergic reaction that can cause a rapid drop in blood pressure, difficulty breathing, and loss of consciousness.
Management of Keflex-Related Allergic Reactions
The management of Keflex-related allergic reactions depends on the severity of the reaction.
- Mild reactions: Mild reactions, such as skin rash or itching, may be treated with antihistamines or topical corticosteroids.
- Severe reactions: Severe reactions, such as swelling, wheezing, or anaphylaxis, require immediate medical attention. Emergency medical personnel will administer epinephrine (adrenaline) to counteract the effects of the allergic reaction. Oxygen may also be provided to assist with breathing.
Cross-Reactivity Between Keflex and Other Penicillin-Class Antibiotics
Keflex belongs to the penicillin class of antibiotics. Individuals who are allergic to one penicillin-class antibiotic may be allergic to others, including Keflex. This is known as cross-reactivity.
Cross-reactivity occurs because penicillin-class antibiotics share a common chemical structure that can trigger an allergic response.
It is essential for healthcare providers to obtain a detailed allergy history from patients, including any previous reactions to penicillin-class antibiotics. This information helps determine the risk of cross-reactivity and guide appropriate antibiotic selection.
Keflex in Clinical Practice
Keflex, also known as cephalexin, is a widely used antibiotic in clinical practice, primarily for treating bacterial infections. Its effectiveness, availability, and generally good safety profile contribute to its widespread use. However, choosing the right antibiotic requires careful consideration of the patient’s condition, potential risks, and the specific bacteria causing the infection.
Clinical Decision-Making Flowchart for Keflex
The decision to use Keflex should involve a systematic approach, considering factors like the type of infection, patient’s allergies, and potential drug interactions. A flowchart can be a helpful tool to guide this process:
- Identify the infection: Determine the type of infection (e.g., skin, respiratory, urinary tract) and the suspected causative organism.
- Assess patient history: Review the patient’s medical history for allergies, especially to penicillin, as cross-reactivity can occur.
- Consider alternative treatments: Evaluate if other antibiotics with a broader spectrum of activity or a more favorable safety profile are more suitable.
- Review drug interactions: Assess for potential interactions with other medications the patient is taking.
- Evaluate renal function: Keflex is primarily excreted by the kidneys, so impaired renal function may require dosage adjustments.
- Monitor patient response: Closely monitor the patient’s response to therapy, including clinical improvement and any potential adverse effects.
Indications, Contraindications, and Precautions
| Category | Details |
|---|---|
| Indications |
|
| Contraindications |
|
| Precautions |
|
Case Studies
Successful Use of Keflex
- Case 1: Skin Infection: A 25-year-old patient presented with a painful, red, and swollen area on her leg consistent with cellulitis. After a culture confirmed Staphylococcus aureus as the causative organism, she was treated with Keflex for 10 days, resulting in complete resolution of the infection.
- Case 2: Otitis Media: A 4-year-old child with recurrent otitis media was diagnosed with Haemophilus influenzae infection. Treatment with Keflex for 7 days effectively cleared the infection, relieving the child’s ear pain and discomfort.
Unsuccessful Use of Keflex
- Case 3: Resistant Strain: A 60-year-old patient with a history of urinary tract infections was prescribed Keflex for a recurrent UTI. However, the infection persisted, and a culture revealed a resistant strain of Escherichia coli, necessitating a change in antibiotic therapy.
- Case 4: Allergic Reaction: A 32-year-old patient with a history of penicillin allergy was prescribed Keflex for a skin infection. Within a few days, she developed a severe rash and itching, prompting discontinuation of the medication and initiation of alternative therapy.
Keflex
Keflex, also known as cephalexin, is a widely prescribed antibiotic that has been a mainstay in the treatment of various bacterial infections for decades. Its effectiveness, safety profile, and ease of administration have contributed to its popularity among healthcare professionals. While Keflex remains a valuable therapeutic option, ongoing research and development efforts are continually exploring its potential and addressing existing challenges.
Future Directions and Research
Ongoing research efforts are focused on enhancing the efficacy and safety of Keflex while exploring new applications. Here are some key areas of investigation:
- Developing Novel Formulations: Research is underway to develop novel formulations of Keflex that improve its bioavailability, reduce dosing frequency, and enhance patient compliance. For example, extended-release formulations are being explored to provide sustained therapeutic levels of the drug over a longer period, reducing the need for multiple daily doses.
- Combating Antibiotic Resistance: The emergence of antibiotic resistance is a significant global health concern. Research is focused on understanding the mechanisms of resistance to Keflex and developing strategies to overcome it. This includes exploring new drug combinations and investigating alternative delivery methods.
- Expanding Therapeutic Applications: Keflex is currently used to treat a wide range of infections. However, ongoing research is exploring its potential in other therapeutic areas, such as the treatment of certain types of cancer and inflammatory diseases. Preclinical studies are investigating the efficacy of Keflex in combination with other therapies for these conditions.
- Personalized Medicine: There is growing interest in tailoring treatment approaches to individual patients based on their genetic makeup and other factors. Research is exploring the use of pharmacogenomics to predict individual responses to Keflex, potentially optimizing treatment outcomes and minimizing adverse effects.
Understanding the intricacies of Keflex is crucial for healthcare professionals and patients alike. By gaining a comprehensive understanding of its properties, applications, and potential risks, we can make informed decisions regarding its use and contribute to responsible antibiotic stewardship. This guide serves as a valuable resource for navigating the complexities of Keflex therapy, promoting safe and effective treatment outcomes.
Keflex, a common antibiotic, is prescribed for various bacterial infections. It’s available in different dosages, and one popular option is the keflex 500 mg dosage. This specific dosage is often used for more severe infections or when a higher concentration of the medication is needed. Keflex, regardless of the dosage, works by inhibiting the growth of bacteria, helping your body fight off the infection.