Nicardipine sets the stage for a comprehensive exploration of a vital calcium channel blocker, offering insights into its chemical structure, pharmacological class, and therapeutic applications. This narrative delves into the intricate mechanism of action, shedding light on how nicardipine interacts with the body to achieve its therapeutic effects.
From its role in managing hypertension and angina to its pharmacokinetic profile, we’ll unravel the intricacies of nicardipine’s journey through the body, including its absorption, distribution, metabolism, and excretion. We’ll also address potential drug interactions, adverse effects, and precautions, providing a comprehensive overview of this important medication.
Nicardipine
Nicardipine is a medication that is primarily used to treat high blood pressure (hypertension). It belongs to a class of drugs known as calcium channel blockers, which work by relaxing the muscles of the blood vessels, allowing blood to flow more easily.
Chemical Structure and Molecular Formula
Nicardipine is a dihydropyridine calcium channel blocker. Its chemical structure is characterized by a 1,4-dihydropyridine ring system.
The molecular formula of nicardipine is C27H32N2O6.
Pharmacological Class
Nicardipine belongs to the class of drugs known as dihydropyridine calcium channel blockers. These drugs work by blocking the influx of calcium ions into smooth muscle cells, specifically in the heart and blood vessels. This mechanism of action leads to relaxation of the smooth muscle cells, resulting in vasodilation (widening of blood vessels).
Mechanism of Action
Nicardipine works by blocking the entry of calcium ions into the smooth muscle cells of blood vessels. Calcium ions are essential for muscle contraction. By inhibiting the entry of calcium ions, nicardipine prevents the smooth muscle cells from contracting, leading to relaxation of the blood vessels. This relaxation of blood vessels lowers blood pressure by reducing the resistance to blood flow.
Therapeutic Applications
Nicardipine is a calcium channel blocker medication primarily used to treat high blood pressure (hypertension) and chest pain (angina). It works by relaxing the blood vessels, which lowers blood pressure and improves blood flow to the heart.
Hypertension
Nicardipine is a highly effective medication for managing hypertension. It helps to lower blood pressure by relaxing the muscles in the walls of blood vessels, which allows blood to flow more easily. The dosage of nicardipine for hypertension varies depending on the individual’s condition and response to treatment.
Nicardipine is typically administered orally in the form of capsules or tablets. The recommended starting dose for most adults is 10 mg taken twice daily. The dose may be increased gradually until the desired blood pressure is achieved.
Angina
Nicardipine is also used to treat angina, a condition that occurs when the heart muscle does not receive enough oxygen. It helps to reduce the frequency and severity of angina episodes by relaxing the blood vessels and improving blood flow to the heart.
Nicardipine is typically administered orally in the form of capsules or tablets. The recommended starting dose for most adults is 10 mg taken twice daily. The dose may be increased gradually until the desired effect is achieved.
Pharmacokinetics and Metabolism
Nicardipine, like other calcium channel blockers, undergoes a series of processes in the body that determine its concentration, duration of action, and potential for interactions with other medications. This section explores the pharmacokinetics of nicardipine, covering its absorption, distribution, metabolism, and excretion. Understanding these processes is crucial for optimizing therapeutic efficacy and minimizing adverse effects.
Absorption
Nicardipine is rapidly and well absorbed after oral administration. Its bioavailability, however, is relatively low, estimated to be around 35% to 50%. This reduced bioavailability is attributed to extensive first-pass metabolism in the liver, where a significant portion of the drug is metabolized before reaching systemic circulation.
Distribution
Once absorbed, nicardipine distributes widely throughout the body, readily crossing the blood-brain barrier. It exhibits a high volume of distribution, suggesting that it readily binds to tissues, particularly to the heart, liver, and kidneys.
Metabolism
Nicardipine undergoes extensive metabolism primarily in the liver, catalyzed by cytochrome P450 (CYP) enzymes. The primary enzyme involved in nicardipine metabolism is CYP3A4, although other CYP enzymes like CYP2D6 and CYP2C9 may also play a role to a lesser extent.
Role of Cytochrome P450 Enzymes
Cytochrome P450 enzymes are a superfamily of enzymes responsible for metabolizing a wide range of drugs and other compounds. CYP3A4, the primary enzyme involved in nicardipine metabolism, is responsible for converting nicardipine into inactive metabolites. This metabolic process is crucial for eliminating nicardipine from the body and preventing its accumulation to toxic levels.
Drug Interactions
The extensive metabolism of nicardipine by CYP3A4 makes it susceptible to drug interactions with other medications that either inhibit or induce this enzyme.
- Inhibitors of CYP3A4, such as ketoconazole, erythromycin, and grapefruit juice, can increase nicardipine plasma concentrations by slowing down its metabolism. This can lead to increased therapeutic effects but also potentially to adverse effects.
- Inducers of CYP3A4, such as rifampin, phenytoin, and carbamazepine, can accelerate nicardipine metabolism, reducing its plasma concentrations and potentially decreasing its therapeutic efficacy.
Therefore, careful monitoring and dose adjustments may be necessary when nicardipine is co-administered with drugs that affect CYP3A4 activity.
Excretion
Nicardipine is primarily excreted in the feces, with a small amount excreted in the urine. The majority of nicardipine is eliminated as inactive metabolites, with only a small fraction of the parent drug excreted unchanged. The elimination half-life of nicardipine is approximately 4 to 6 hours, suggesting that its effects typically last for several hours.
Adverse Effects and Precautions
Nicardipine, like many medications, can cause adverse effects. These effects can range from mild and manageable to serious and potentially life-threatening. It’s crucial to understand these potential risks and take necessary precautions to minimize them.
Common Adverse Effects, Nicardipine
Common adverse effects of nicardipine are usually mild and tend to subside with continued use. They include:
- Headache
- Dizziness
- Flushing
- Nausea
- Peripheral edema (swelling in the legs and feet)
If these effects persist or worsen, consult your healthcare provider.
Serious Adverse Effects
While less common, nicardipine can also cause serious adverse effects. These require immediate medical attention:
- Hypotension (low blood pressure): This can lead to dizziness, fainting, and even shock.
- Bradycardia (slow heart rate): This can be dangerous, especially in individuals with pre-existing heart conditions.
- Hepatic dysfunction (liver problems): Symptoms may include jaundice (yellowing of the skin and eyes), abdominal pain, and dark urine.
- Angina (chest pain): Nicardipine can sometimes worsen angina symptoms in individuals with coronary artery disease.
It’s important to be aware of these potential risks and seek immediate medical attention if you experience any of these symptoms while taking nicardipine.
Contraindications
Nicardipine is contraindicated in certain situations, meaning it should not be used. These include:
- Hypersensitivity (allergy) to nicardipine or any of its ingredients.
- Severe aortic stenosis (narrowing of the aortic valve): Nicardipine can worsen this condition.
- Unstable angina (chest pain that occurs at rest or with minimal exertion): Nicardipine may not be effective in this situation.
- Pregnancy and breastfeeding: Nicardipine can cross the placenta and enter breast milk, potentially harming the fetus or infant.
It’s crucial to inform your healthcare provider about any allergies or pre-existing medical conditions before starting nicardipine therapy.
Monitoring Blood Pressure and Heart Rate
Regular monitoring of blood pressure and heart rate is essential during nicardipine therapy. This is because nicardipine can cause significant drops in blood pressure and changes in heart rate.
- Blood pressure monitoring: Blood pressure should be monitored regularly, both at home and during office visits. This helps ensure that the dosage is appropriate and that the medication is effective.
- Heart rate monitoring: Heart rate should also be monitored regularly. If your heart rate becomes too slow, your healthcare provider may need to adjust your dosage or consider alternative medications.
It’s important to follow your healthcare provider’s instructions carefully and report any changes in your blood pressure or heart rate.
Nicardipine and Pregnancy

Nicardipine, a calcium channel blocker, is used to treat high blood pressure and chest pain (angina). While effective in many cases, its use during pregnancy raises concerns about potential risks to the developing fetus.
Safety During Pregnancy and Breastfeeding
The safety of nicardipine during pregnancy has not been fully established. Studies in animals have shown adverse effects on the fetus, including decreased fetal weight and skeletal abnormalities. However, limited human data suggests that nicardipine may not pose significant risks to the fetus when used during pregnancy.
It is crucial to weigh the potential benefits of nicardipine therapy against the potential risks for both the mother and the fetus. The decision to use nicardipine during pregnancy should be made on a case-by-case basis, considering the individual patient’s medical history and the severity of their condition.
Nicardipine is excreted in breast milk. It is unknown whether it can harm a nursing infant. Therefore, breastfeeding is not recommended while taking nicardipine.
Nicardipine in Clinical Practice
Nicardipine is a widely used calcium channel blocker for the treatment of hypertension and angina. Its effectiveness and safety profile have made it a mainstay in clinical practice. Understanding the different formulations, potential drug interactions, and management strategies for patients on nicardipine therapy is crucial for healthcare professionals.
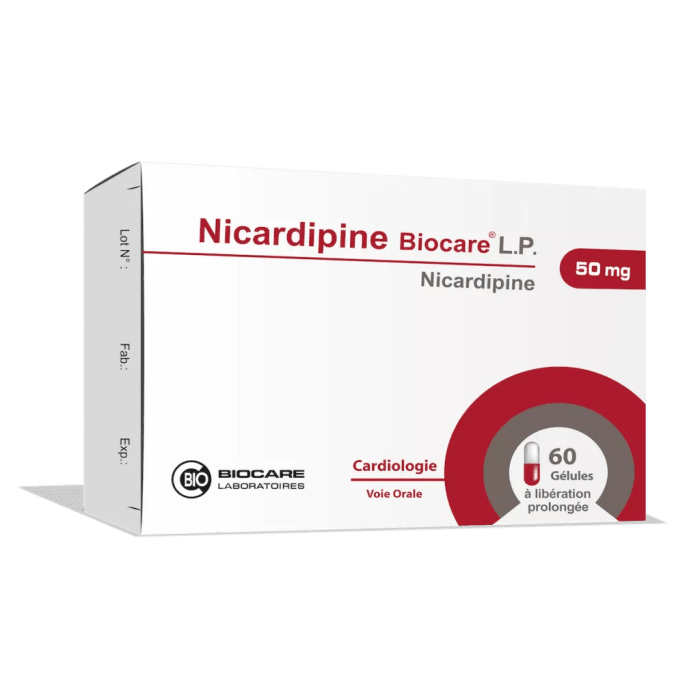
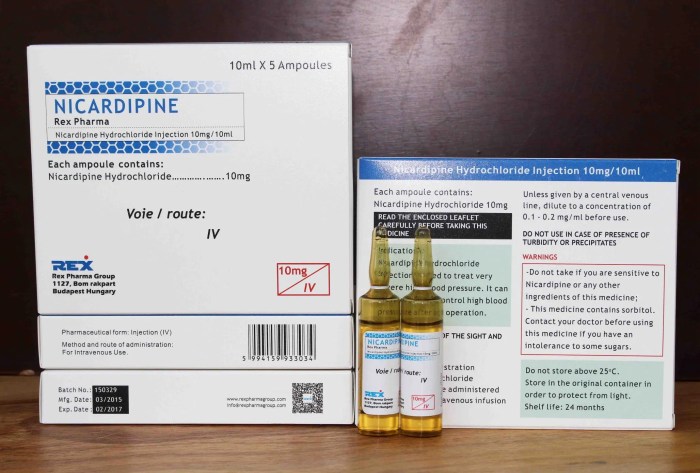
Formulations of Nicardipine
Nicardipine is available in various formulations to suit different patient needs and preferences.
| Formulation | Route of Administration | Dosage |
|---|---|---|
| Nicardipine capsules | Oral | 10 mg, 20 mg, 30 mg |
| Nicardipine extended-release capsules | Oral | 20 mg, 30 mg, 40 mg, 60 mg |
| Nicardipine intravenous injection | Intravenous | 2.5 mg/mL, 5 mg/mL |
Drug Interactions with Nicardipine
Nicardipine can interact with various drugs, potentially altering its efficacy or increasing the risk of adverse effects.
| Drug Class | Drug Examples | Potential Interaction |
|---|---|---|
| Other calcium channel blockers | Verapamil, diltiazem | Increased risk of bradycardia, hypotension |
| Beta-blockers | Propranolol, metoprolol | Additive negative inotropic effects, bradycardia |
| Grapefruit juice | N/A | Increased nicardipine levels, potential for toxicity |
| Statins | Simvastatin, atorvastatin | Increased risk of myopathy |
| CYP3A4 inhibitors | Ketoconazole, erythromycin | Increased nicardipine levels, potential for toxicity |
Management of Nicardipine Therapy
Effective management of patients on nicardipine therapy involves a comprehensive approach.
Flowchart: Management of Nicardipine Therapy
[Flowchart:
– Start
– Assess patient’s medical history, current medications, and any allergies.
– Initiate nicardipine therapy with appropriate dosage and formulation based on patient’s condition.
– Monitor blood pressure and heart rate regularly.
– Adjust dosage as needed based on clinical response and adverse effects.
– Educate patient about nicardipine therapy, including potential side effects and interactions.
– Regularly monitor for potential adverse effects and adjust therapy accordingly.
– Follow-up with patient to ensure optimal therapeutic outcomes.
– End]
Research and Development
Nicardipine, a calcium channel blocker, has a well-established role in the treatment of hypertension and angina. However, ongoing research continues to explore new applications and refine its use in various clinical settings.
Ongoing Research and Clinical Trials
Research efforts are underway to investigate the potential benefits of nicardipine in diverse medical fields. Several clinical trials are actively evaluating the efficacy and safety of nicardipine for conditions beyond its traditional indications.
- Neurological Disorders: Studies are investigating the potential of nicardipine in managing neurological conditions such as stroke, subarachnoid hemorrhage, and traumatic brain injury. Preliminary findings suggest that nicardipine may have neuroprotective effects, potentially reducing neurological damage and improving functional outcomes. For example, a study published in the journal “Stroke” in 2019 explored the use of nicardipine in patients with acute ischemic stroke. The study found that nicardipine administration within 24 hours of stroke onset was associated with improved neurological function and a lower risk of death.
- Cancer: Emerging research is exploring the potential of nicardipine in cancer therapy. Some studies suggest that nicardipine may inhibit tumor growth and angiogenesis (the formation of new blood vessels that supply tumors) in certain types of cancer. For instance, a study published in the journal “Cancer Research” in 2020 investigated the effects of nicardipine on breast cancer cell lines. The study demonstrated that nicardipine significantly inhibited the growth and proliferation of breast cancer cells, suggesting its potential as a novel therapeutic agent.
- Cardiovascular Disease: Nicardipine’s potential in treating heart failure and preventing heart attacks is being investigated. Some research suggests that nicardipine might improve cardiac function and reduce the risk of cardiovascular events in patients with heart failure. For example, a study published in the journal “Circulation” in 2018 evaluated the effects of nicardipine on patients with chronic heart failure. The study found that nicardipine was associated with improved left ventricular function and a reduced incidence of hospitalization for heart failure.
Future Directions for Nicardipine Research
The future of nicardipine research holds promising possibilities for expanding its therapeutic applications and improving patient care.
- Combination Therapies: Research is exploring the potential of combining nicardipine with other medications to enhance its therapeutic effects. For instance, combining nicardipine with other antihypertensive drugs may lead to improved blood pressure control and a reduced risk of cardiovascular events.
- Targeted Drug Delivery: Research is focusing on developing targeted drug delivery systems to enhance the effectiveness of nicardipine and minimize its side effects. This approach aims to deliver the drug directly to the target tissues, reducing systemic exposure and potential adverse reactions. For example, research is exploring the use of nanoparticles to encapsulate nicardipine and target specific organs or tissues.
- Personalized Medicine: Advances in personalized medicine are leading to the development of pharmacogenomic tests that can identify patients who are most likely to benefit from nicardipine therapy. This approach aims to optimize drug selection and dosage based on individual genetic variations.
Nicardipine vs. Other Calcium Channel Blockers
Nicardipine is a calcium channel blocker that is commonly used to treat hypertension and angina. It is a member of the dihydropyridine class of calcium channel blockers, which also includes nifedipine, amlodipine, and felodipine. These medications work by blocking the entry of calcium into the heart muscle and blood vessels, which helps to relax the muscles and lower blood pressure. Nicardipine is typically administered orally, but it is also available in an intravenous formulation.
Clinical Scenarios for Nicardipine vs. Other Calcium Channel Blockers
The choice of calcium channel blocker for a particular patient will depend on a number of factors, including the patient’s medical history, the severity of their condition, and their tolerance to different medications. Nicardipine, nifedipine, amlodipine, and felodipine have distinct pharmacokinetic profiles and clinical applications.
- Nicardipine: Nicardipine is often preferred for patients with Prinzmetal’s angina (variant angina) because it has a rapid onset of action and a relatively short half-life. It is also commonly used for patients with hypertension who have a history of coronary artery disease.
- Nifedipine: Nifedipine is available in immediate-release and sustained-release formulations. The immediate-release formulation is used for the acute treatment of angina, while the sustained-release formulation is used for the long-term management of hypertension.
- Amlodipine: Amlodipine has a long half-life, making it a good choice for patients who need a once-daily medication. It is also a good option for patients with hypertension who have a history of coronary artery disease.
- Felodipine: Felodipine is a long-acting calcium channel blocker that is typically used for the long-term management of hypertension. It is available in a sustained-release formulation that is taken once daily.
Patient Education and Counseling
It’s crucial for patients starting nicardipine therapy to understand the medication’s purpose, potential benefits, and potential risks. Open communication between patients and healthcare providers is essential for successful treatment.
Understanding Nicardipine
Patients should be informed about the purpose of nicardipine, which is to relax blood vessels and lower blood pressure. They should understand that nicardipine is a calcium channel blocker, a class of medications that work by blocking the entry of calcium into the heart and blood vessels.
Importance of Adherence
Adherence to the prescribed dosage and schedule is crucial for the effectiveness of nicardipine therapy. Patients should be informed about the following:
- Taking nicardipine exactly as prescribed by their doctor, including the dosage, frequency, and timing of doses.
- Not stopping nicardipine abruptly without consulting their doctor, as this could lead to a sudden increase in blood pressure.
- Avoiding missed doses, as this could reduce the effectiveness of the medication.
- Keeping a record of their medication intake and any side effects experienced.
Monitoring for Side Effects
Patients should be aware of potential side effects of nicardipine and know how to monitor for and manage them. Common side effects include:
- Headache
- Dizziness
- Flushing
- Swelling in the ankles and feet
- Constipation
Patients should be advised to contact their doctor immediately if they experience any serious side effects, such as:
- Chest pain
- Shortness of breath
- Irregular heartbeat
- Swelling of the face, lips, tongue, or throat
- Difficulty swallowing
- Skin rash or itching
- Yellowing of the skin or eyes
- Dark urine
- Unusual bleeding or bruising
Conclusion
Nicardipine stands as a valuable therapeutic option for managing hypertension and angina, offering a range of benefits, including efficacy in reducing blood pressure and improving heart function. Its unique pharmacokinetic profile, with a rapid onset and short duration of action, allows for flexible dosing and individualized treatment strategies. However, like all medications, nicardipine has its limitations, including potential adverse effects and drug interactions.
The understanding of nicardipine’s therapeutic profile continues to evolve with ongoing research and development. Further investigations into its potential applications, particularly in managing specific patient populations and exploring novel drug delivery systems, are crucial for optimizing its clinical utility.
As we conclude our exploration of nicardipine, we are left with a deeper understanding of this crucial calcium channel blocker, appreciating its diverse therapeutic applications and the importance of careful monitoring during therapy. The ongoing research and development surrounding nicardipine hold promising potential for expanding its clinical use and improving patient outcomes. Through continued exploration and understanding, we can harness the therapeutic power of nicardipine to improve the lives of individuals seeking effective management of cardiovascular conditions.
Nicardipine, a calcium channel blocker, is often used to manage high blood pressure. While it primarily targets the cardiovascular system, its effects can sometimes extend to other areas, such as mood regulation. This is where a drug like vortioxetine , a serotonin modulator, might come into play. Vortioxetine, known for its impact on mood and cognition, could potentially complement nicardipine’s effects, offering a more comprehensive approach to managing certain conditions.