Ramipril, a widely prescribed medication, stands as a cornerstone in the management of high blood pressure. It belongs to a class of drugs known as angiotensin-converting enzyme (ACE) inhibitors, working to relax blood vessels and improve blood flow.
This drug’s mechanism of action centers around inhibiting the production of angiotensin II, a potent vasoconstrictor. By blocking ACE, ramipril effectively reduces blood pressure, easing the strain on the heart and preventing complications associated with hypertension.
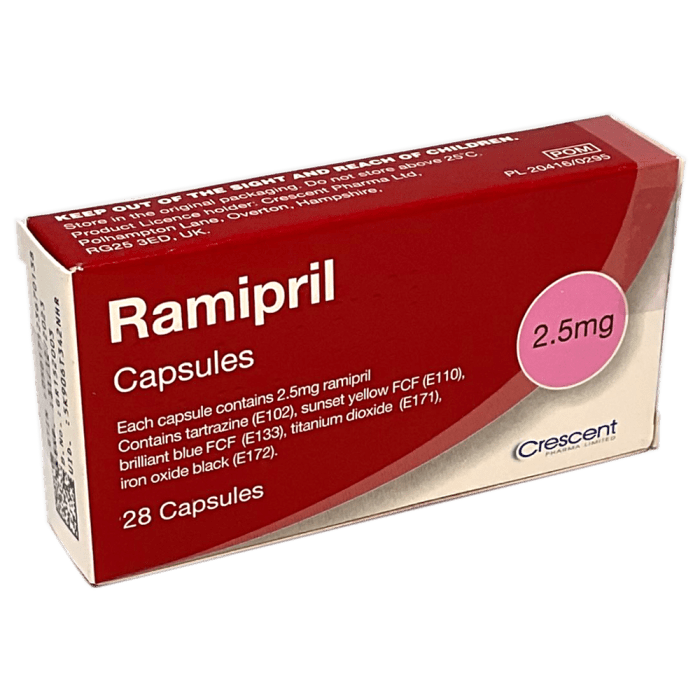
Ramipril
Ramipril is a medication that belongs to a group of drugs called angiotensin-converting enzyme (ACE) inhibitors. It is commonly prescribed for the treatment of high blood pressure (hypertension) and heart failure. It works by relaxing blood vessels, which lowers blood pressure and reduces the workload on the heart.
Ramipril: An Overview
Ramipril is a synthetically produced drug with the chemical structure and molecular formula:
C15H21N3O5

Ramipril belongs to the drug family of ACE inhibitors. These drugs work by blocking the action of an enzyme called angiotensin-converting enzyme (ACE). ACE is responsible for converting angiotensin I to angiotensin II, a powerful vasoconstrictor that raises blood pressure. By inhibiting ACE, ramipril prevents the formation of angiotensin II, leading to vasodilation (relaxation of blood vessels) and a reduction in blood pressure.
Medical Applications

Ramipril is a widely prescribed medication used to treat a variety of cardiovascular conditions. Its effectiveness stems from its ability to block the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. This mechanism of action results in vasodilation, reduced blood pressure, and a decrease in the workload of the heart.
Hypertension
Ramipril is a cornerstone medication for the management of hypertension, both as monotherapy and in combination with other antihypertensive drugs. It effectively lowers blood pressure by relaxing blood vessels, allowing blood to flow more easily.
- Ramipril reduces the risk of stroke, heart attack, and heart failure in patients with hypertension.
- Long-term use of ramipril has been shown to improve cardiovascular outcomes in patients with hypertension.
Heart Failure
Ramipril is a vital component of heart failure treatment, particularly in patients with reduced ejection fraction. Its vasodilatory properties alleviate the burden on the heart, improving its ability to pump blood effectively.
- Ramipril reduces the risk of hospitalization and mortality in patients with heart failure.
- It improves symptoms such as shortness of breath, fatigue, and swelling in the legs and ankles.
Post-Myocardial Infarction
After a heart attack, ramipril plays a crucial role in reducing the risk of subsequent cardiovascular events. Its ability to lower blood pressure and improve heart function helps prevent further damage to the heart.
- Ramipril has been shown to reduce the risk of death, heart attack, and stroke in patients who have had a heart attack.
- It improves the survival rate and quality of life for patients who have experienced a myocardial infarction.
Diabetic Nephropathy
Ramipril is an effective medication for slowing the progression of diabetic nephropathy, a complication of diabetes that affects the kidneys. It reduces the amount of protein in the urine, a marker of kidney damage.
- Ramipril slows the decline in kidney function and reduces the risk of needing dialysis.
- It has been shown to improve the survival rate in patients with diabetic nephropathy.
Combination Therapies
Ramipril is frequently used in combination with other medications to manage cardiovascular conditions.
- For hypertension, ramipril is often combined with diuretics, beta-blockers, or calcium channel blockers to achieve optimal blood pressure control.
- In heart failure, ramipril is frequently combined with beta-blockers, diuretics, and digoxin to improve heart function and reduce symptoms.
Dosage and Administration
Ramipril is available in various forms and dosages, tailored to the individual’s condition and needs. The physician carefully determines the appropriate dosage, considering factors like age, weight, and kidney function.
Dosage Range
The starting dosage of ramipril usually ranges from 1.25 mg to 2.5 mg once daily. This dosage may be adjusted based on the patient’s response to treatment.
For example, for hypertension, the typical starting dosage is 2.5 mg once daily. This dosage may be increased gradually, depending on the blood pressure control achieved. In patients with heart failure, the initial dosage is usually 1.25 mg once daily, which can be increased to a maximum of 10 mg daily, depending on individual tolerance and response.
Routes of Administration
Ramipril is typically administered orally, with tablets being the most common form. The tablets are usually swallowed whole with water.
Frequency and Duration of Treatment, Ramipril
The frequency of ramipril administration is typically once daily. The duration of treatment is determined by the physician and depends on the underlying condition being treated.
For example, in patients with hypertension, ramipril treatment is usually lifelong to maintain blood pressure control. In patients with heart failure, the duration of treatment is also generally long-term, as it helps improve heart function and reduce the risk of future heart events.
Side Effects and Precautions
Ramipril, like most medications, can cause side effects. While most side effects are mild and temporary, some can be serious. Understanding the potential side effects and precautions is crucial for safe and effective use of ramipril.
Common Side Effects
Common side effects of ramipril are generally mild and usually resolve on their own within a few days or weeks.
- Cough: This is a common side effect, particularly in the early stages of treatment. It is usually mild and tends to improve over time.
- Dizziness: This can occur due to a drop in blood pressure, especially when standing up quickly.
- Headache: This is a common side effect, particularly in the early stages of treatment.
- Fatigue: This is a common side effect, particularly in the early stages of treatment.
Serious Side Effects
While rare, ramipril can cause serious side effects. It is important to seek immediate medical attention if you experience any of the following:
- Angioedema: This is a serious allergic reaction that causes swelling of the face, lips, tongue, and throat. It can be life-threatening and requires immediate medical attention.
- Hypotension: This is a significant drop in blood pressure that can cause dizziness, fainting, and even shock.
- Kidney problems: Ramipril can sometimes cause kidney problems, especially in people with pre-existing kidney disease.
- Elevated potassium levels: Ramipril can increase potassium levels in the blood, which can be dangerous for people with kidney disease or other medical conditions.
Contraindications and Precautions
Ramipril is not suitable for everyone. It is important to inform your doctor about your medical history, including any allergies, current medications, and pre-existing conditions.
- Pregnancy and breastfeeding: Ramipril is not recommended for use during pregnancy or breastfeeding.
- Kidney disease: Ramipril should be used with caution in people with kidney disease.
- Liver disease: Ramipril should be used with caution in people with liver disease.
- Diabetes: Ramipril can affect blood sugar levels, so it should be used with caution in people with diabetes.
- Surgery: Ramipril should be stopped a few days before surgery.
Interactions with Other Medications
Ramipril, like many other medications, can interact with other drugs, potentially altering their effectiveness or increasing the risk of side effects. Understanding these interactions is crucial for safe and effective treatment.
Potential Drug Interactions
It is essential to be aware of potential drug interactions with ramipril. These interactions can occur due to various mechanisms, such as:
- Competition for the same metabolic pathway: Some medications might compete with ramipril for the same enzymes responsible for breaking down drugs in the body. This competition can lead to increased levels of either drug, potentially causing adverse effects.
- Altered renal function: Ramipril can affect kidney function, which can impact the elimination of other medications from the body. This can result in higher drug levels and an increased risk of side effects.
- Additive effects: Some medications, when combined with ramipril, can have additive effects, increasing the risk of certain side effects, such as hypotension or hyperkalemia.
Examples of Medications to Avoid with Ramipril
Here are some examples of medications that should be avoided or used with caution when taking ramipril:
- Potassium-sparing diuretics (e.g., spironolactone, amiloride): These drugs can increase potassium levels in the blood, which can be exacerbated by ramipril, potentially leading to hyperkalemia.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., ibuprofen, naproxen): NSAIDs can reduce the effectiveness of ramipril by interfering with its ability to lower blood pressure. They can also increase the risk of kidney problems.
- Lithium: Ramipril can increase lithium levels in the blood, potentially leading to lithium toxicity.
- Anti-diabetic medications (e.g., insulin, sulfonylureas): Ramipril can increase the risk of hypoglycemia when combined with these medications.
- Anesthetics: Ramipril can enhance the effects of anesthetics, potentially leading to hypotension and bradycardia.
Ramipril and Pregnancy
Ramipril, an ACE inhibitor, is not recommended for use during pregnancy. It is categorized as a pregnancy category D drug, meaning that there is positive evidence of human fetal risk. This means that the potential benefits of using ramipril during pregnancy do not outweigh the risks to the developing fetus.
Potential Risks to the Fetus
The use of ramipril during pregnancy has been linked to several potential risks to the fetus, including:
- Fetal death: In some cases, the use of ramipril during pregnancy has been associated with fetal death. The exact mechanisms by which ramipril might cause fetal death are not fully understood, but it is believed to be related to its effects on the fetal circulatory system.
- Birth defects: Ramipril may increase the risk of birth defects, such as:
- Renal defects: Ramipril can affect the development of the fetal kidneys, potentially leading to kidney problems in the newborn.
- Skeletal defects: Ramipril may also affect the development of the fetal skeleton, leading to skeletal abnormalities.
- Craniofacial defects: Ramipril may also contribute to craniofacial abnormalities in the newborn.
- Premature birth: Ramipril may increase the risk of premature birth, which can lead to various health complications for the newborn.
- Low birth weight: The use of ramipril during pregnancy may also lead to babies being born with low birth weight, which can increase the risk of health problems in the newborn.
- Fetal hypotension: Ramipril can cause fetal hypotension (low blood pressure), which can be dangerous for the developing fetus.
Ramipril and Kidney Function

Ramipril, an angiotensin-converting enzyme (ACE) inhibitor, can have a significant impact on kidney function. Its ability to lower blood pressure and reduce the workload on the heart can also benefit the kidneys. However, it’s crucial to understand the potential effects of ramipril on kidney health and how to manage them effectively.
Ramipril’s Impact on Kidney Function
Ramipril can have a protective effect on the kidneys in individuals with pre-existing kidney disease or those at risk of developing kidney problems. This is because ramipril helps to:
- Reduce blood pressure, which decreases the pressure on the kidneys.
- Dilate blood vessels, improving blood flow to the kidneys.
- Block the production of angiotensin II, a hormone that constricts blood vessels and can damage the kidneys.
However, in some cases, ramipril can also lead to a decline in kidney function. This is more likely to occur in individuals with severe kidney disease, those who are dehydrated, or those taking other medications that can affect kidney function.
Ramipril in Patients with Pre-existing Kidney Disease
Ramipril can be used cautiously in patients with pre-existing kidney disease. The decision to use ramipril in these individuals should be made on a case-by-case basis, considering the severity of the kidney disease and the potential benefits and risks.
Monitoring Kidney Function During Ramipril Therapy
Regular monitoring of kidney function is essential during ramipril therapy, especially in patients with pre-existing kidney disease or those at risk of developing kidney problems. This monitoring typically involves:
- Checking serum creatinine levels, a measure of kidney function.
- Monitoring urine output.
- Assessing for any signs or symptoms of kidney dysfunction, such as swelling in the legs or feet, fatigue, or shortness of breath.
If any signs of kidney dysfunction are detected, the dosage of ramipril may need to be adjusted or the medication may need to be discontinued.
Ramipril, a valuable tool in the fight against hypertension, offers a comprehensive approach to managing blood pressure. Its effectiveness, coupled with a well-established safety profile, makes it a mainstay in the treatment of various cardiovascular conditions. Understanding its mechanism of action, potential side effects, and interactions is crucial for maximizing its benefits and ensuring safe and effective use.
Ramipril is a medication commonly used to treat high blood pressure and heart failure. It works by relaxing blood vessels, which helps lower blood pressure. While ramipril focuses on the cardiovascular system, lamivudine is a medication used to treat viral infections, specifically HIV and hepatitis B. Both medications are important for managing their respective conditions and improving overall health.