Rituximab, a groundbreaking monoclonal antibody, has revolutionized the treatment of various autoimmune and hematological malignancies. This targeted therapy selectively binds to CD20, a protein found on the surface of B lymphocytes, effectively depleting these cells from the body. By interfering with the immune system’s B cells, rituximab has proven effective in managing conditions like rheumatoid arthritis, lupus, lymphoma, and leukemia.
Rituximab’s mechanism of action involves targeting the CD20 antigen present on B lymphocytes. It binds to CD20, triggering a cascade of events that ultimately lead to the destruction of B cells. This selective targeting allows rituximab to effectively reduce the immune system’s attack on healthy tissues in autoimmune disorders and eliminate cancerous B cells in hematological malignancies. Its administration involves intravenous infusions, with dosage regimens varying depending on the specific condition and patient factors.
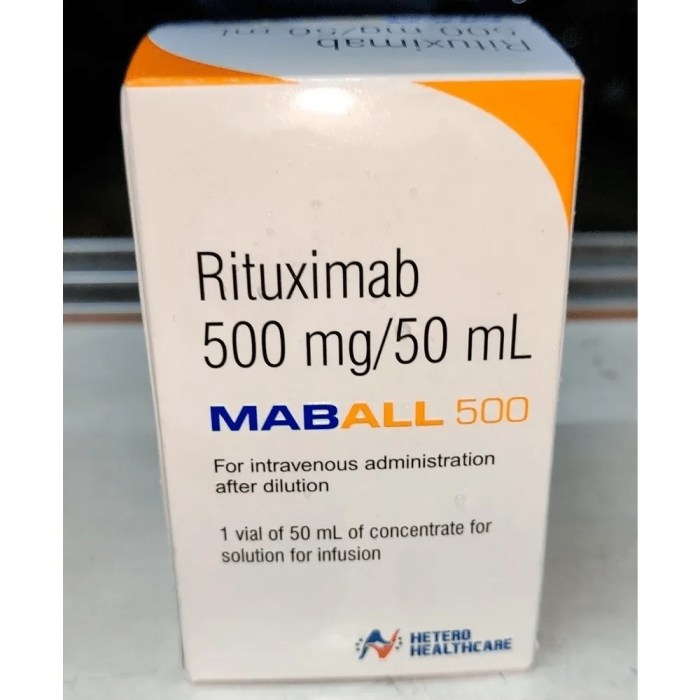
Rituximab
Rituximab is a monoclonal antibody medication used to treat various cancers and autoimmune diseases. It is classified as a therapeutic antibody, a type of medication that targets specific cells or proteins in the body.
Mechanism of Action
Rituximab works by targeting a specific protein called CD20, which is found on the surface of B cells. B cells are a type of white blood cell that plays a crucial role in the immune system. Rituximab binds to CD20, leading to the destruction of B cells through several mechanisms, including:
* Complement-dependent cytotoxicity (CDC): Rituximab binds to CD20, attracting complement proteins, which trigger the destruction of B cells.
* Antibody-dependent cell-mediated cytotoxicity (ADCC): Rituximab binds to CD20, attracting natural killer (NK) cells, which then kill the B cells.
* Direct apoptosis: Rituximab can directly induce B cell death by triggering programmed cell death (apoptosis).
By reducing the number of B cells, rituximab can suppress the immune system and effectively treat various conditions.
Chemical Structure and Formulation
Rituximab is a chimeric monoclonal antibody, meaning it is composed of both human and mouse antibody components. Its chemical structure consists of a heavy chain and a light chain, each with a variable region that specifically recognizes and binds to CD20. The variable region is linked to a constant region, which determines the antibody’s effector function.
Rituximab is available in a pharmaceutical formulation as a sterile, preservative-free, lyophilized (freeze-dried) powder for intravenous (IV) administration. It is typically reconstituted with sterile water for injection before administration.
Therapeutic Applications of Rituximab
Rituximab, a monoclonal antibody, has revolutionized the treatment of various diseases by targeting the CD20 antigen found on the surface of B lymphocytes. Its therapeutic applications extend across a wide spectrum of conditions, primarily in autoimmune disorders and hematological malignancies.
Autoimmune Disorders
Rituximab’s role in managing autoimmune disorders stems from its ability to deplete B cells, which are implicated in the pathogenesis of these conditions. The depletion of B cells helps to reduce the production of autoantibodies, thereby mitigating the inflammatory response that characterizes autoimmune diseases.
Rheumatoid Arthritis
Rituximab is a valuable treatment option for rheumatoid arthritis (RA), particularly for patients who have not responded adequately to conventional therapies. It is typically used in combination with methotrexate, a disease-modifying antirheumatic drug (DMARD).
- In RA, Rituximab targets B cells that produce autoantibodies, like rheumatoid factor and anti-citrullinated protein antibodies (ACPA), which contribute to joint inflammation and damage.
- Studies have shown that Rituximab can significantly improve clinical outcomes in RA, including reducing joint swelling, pain, and disease activity.
- The benefits of Rituximab in RA are typically observed within a few weeks of treatment initiation and can last for several months.
Systemic Lupus Erythematosus
Rituximab is also being investigated as a potential treatment for systemic lupus erythematosus (SLE), another autoimmune disorder.
- SLE is characterized by the production of autoantibodies that target various organs and tissues, leading to inflammation and damage.
- Clinical trials have demonstrated that Rituximab can improve disease activity and reduce the need for corticosteroids in patients with SLE.
- However, further research is needed to establish the long-term efficacy and safety of Rituximab in SLE.
Hematological Malignancies
Rituximab has emerged as a cornerstone of treatment for various hematological malignancies, particularly lymphomas and leukemias.
Non-Hodgkin Lymphoma
Rituximab is widely used in the treatment of non-Hodgkin lymphoma (NHL), a type of cancer that affects the lymphatic system.
- Rituximab is often combined with chemotherapy to achieve better outcomes in NHL patients.
- It can be used as a single agent or in combination with other therapies, depending on the type and stage of NHL.
- Rituximab has significantly improved survival rates for NHL patients, particularly those with aggressive forms of the disease.
Chronic Lymphocytic Leukemia
Rituximab is also approved for the treatment of chronic lymphocytic leukemia (CLL), a type of cancer that affects the B cells in the blood and bone marrow.
- Rituximab is typically used in combination with chemotherapy to target and destroy CLL cells.
- It has demonstrated significant efficacy in reducing the number of CLL cells and improving patient survival.
- Rituximab is often considered a first-line treatment option for CLL patients.
Rituximab Administration and Dosing
Rituximab is typically administered intravenously, usually as an infusion. This method allows for controlled and gradual delivery of the drug into the bloodstream, minimizing the risk of adverse effects.
Dosage Regimens
Dosage regimens for rituximab vary depending on the specific condition being treated. Here’s a general overview of typical dosage regimens for different conditions:
- Non-Hodgkin’s Lymphoma (NHL): The initial dosage for NHL is usually 375 mg/m2 administered intravenously over 4 hours on days 1 and 8 of a 21-day cycle. Subsequent cycles may use a reduced dosage of 375 mg/m2 on day 1 only. The total number of cycles varies depending on the specific NHL subtype and the patient’s response to treatment.
- Rheumatoid Arthritis (RA): For RA, the typical dosage is 1000 mg administered intravenously over 4 hours. This dose is usually given on days 1 and 15 of a 21-day cycle. Subsequent cycles may be administered at 2-month intervals, depending on the patient’s response to treatment.
- Other Conditions: Dosage regimens for other conditions, such as granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA), are tailored to the specific disease and patient characteristics.
Factors Influencing Rituximab Dosage
Several factors can influence the dosage of rituximab, including:
- Patient Weight: Rituximab dosage is often calculated based on the patient’s body surface area (BSA), which is a measure of their size. BSA is typically calculated using a formula that takes into account the patient’s height and weight.
- Disease Severity: Patients with more severe disease may require higher doses of rituximab to achieve a therapeutic response. For example, patients with aggressive NHL may receive higher doses than those with indolent NHL.
- Prior Treatment History: Patients who have previously received rituximab or other chemotherapy agents may have different responses to treatment, which may affect the dosage regimen.
- Kidney Function: Rituximab is primarily eliminated by the kidneys. Patients with impaired kidney function may require lower doses or more frequent monitoring to prevent drug accumulation.
- Liver Function: Rituximab is metabolized by the liver. Patients with impaired liver function may require lower doses or more frequent monitoring to prevent drug accumulation.
Pharmacokinetic Properties of Rituximab
Rituximab’s pharmacokinetic profile is crucial for understanding its therapeutic effects and potential side effects. This section will delve into the absorption, distribution, metabolism, and excretion of rituximab in the body, exploring factors influencing its pharmacokinetic behavior.
Half-Life of Rituximab
The half-life of rituximab, the time it takes for the drug concentration in the body to reduce by half, is approximately 5 days. However, this can vary depending on several factors, including the dose administered, the route of administration, and the patient’s individual characteristics. The prolonged half-life of rituximab contributes to its long-lasting therapeutic effect, as it allows for sustained depletion of B cells even after a single infusion.
Potential for Drug Interactions
Rituximab’s potential for drug interactions is a significant consideration in clinical practice. Rituximab can interact with other medications, potentially affecting their efficacy or increasing the risk of adverse effects. For instance, rituximab can enhance the immunosuppressive effects of other drugs, such as corticosteroids or other cytotoxic agents, increasing the risk of infections.
Factors Influencing the Pharmacokinetic Profile of Rituximab
Several factors can influence the pharmacokinetic profile of rituximab, including:
- Dose: Higher doses of rituximab generally lead to higher peak plasma concentrations and longer half-lives.
- Route of Administration: Rituximab is typically administered intravenously, and its pharmacokinetic profile may differ with other routes of administration.
- Patient Characteristics: Factors such as age, weight, renal function, and hepatic function can influence the pharmacokinetic profile of rituximab. For example, patients with impaired renal function may experience slower elimination of rituximab, leading to higher drug levels in the body.
Efficacy and Safety of Rituximab
Rituximab has demonstrated significant efficacy in various hematological malignancies and autoimmune disorders. Its effectiveness stems from its ability to target and deplete B cells, which play a crucial role in the pathogenesis of these conditions. However, like all medications, rituximab is associated with potential adverse effects, some of which can be serious. This section will delve into the clinical evidence supporting rituximab’s efficacy and examine the safety profile of this important therapeutic agent.
Clinical Evidence of Efficacy
Rituximab has been extensively studied in clinical trials, demonstrating its efficacy in a wide range of conditions. The following are some key examples:
- Non-Hodgkin’s Lymphoma (NHL): Rituximab is a cornerstone of treatment for various NHL subtypes, including follicular lymphoma, mantle cell lymphoma, and diffuse large B-cell lymphoma. In combination with chemotherapy, rituximab has been shown to significantly improve response rates, progression-free survival, and overall survival in patients with NHL.
- Chronic Lymphocytic Leukemia (CLL): Rituximab is also effective in the treatment of CLL, both as a single agent and in combination with other therapies. Studies have demonstrated that rituximab can improve response rates, time to progression, and overall survival in patients with CLL.
- Rheumatoid Arthritis (RA): Rituximab is a valuable treatment option for patients with RA who have not responded adequately to conventional therapies. It targets B cells, which are known to play a role in the inflammation and joint damage associated with RA. Clinical trials have shown that rituximab can significantly reduce disease activity, improve joint function, and slow the progression of joint damage in patients with RA.
- Other Autoimmune Disorders: Rituximab has also been investigated for the treatment of other autoimmune disorders, including systemic lupus erythematosus (SLE), vasculitis, and inflammatory bowel disease (IBD). While its efficacy in these conditions is still under investigation, preliminary data suggest that rituximab may be beneficial in some patients.
Common Adverse Effects, Rituximab
Rituximab is generally well-tolerated, but it can cause a range of adverse effects, some of which can be serious.
- Infusion Reactions: Infusion reactions are a common side effect of rituximab. These reactions can range from mild symptoms, such as fever, chills, and headache, to more severe reactions, such as hypotension, bronchospasm, and anaphylaxis. It is crucial to monitor patients closely during and after rituximab infusions to detect and manage any potential infusion reactions.
- Infections: Rituximab depletes B cells, which are important for immune function. This can increase the risk of infections, including bacterial, viral, and fungal infections. Patients receiving rituximab should be monitored for signs and symptoms of infection, and appropriate prophylactic measures may be necessary.
- Hematologic Toxicity: Rituximab can also cause hematologic toxicity, such as neutropenia (low white blood cell count) and thrombocytopenia (low platelet count). These effects are usually mild and transient but can be serious in some cases.
- Other Adverse Effects: Other adverse effects associated with rituximab include fatigue, nausea, vomiting, diarrhea, rash, and liver enzyme elevations.
Serious Adverse Events
While rituximab is generally safe, there is a potential for serious adverse events.
- Infusion Reactions: As mentioned previously, infusion reactions can be serious, even life-threatening.
- Infections: Serious infections, including pneumonia, sepsis, and meningitis, can occur in patients receiving rituximab.
- Progressive Multifocal Leukoencephalopathy (PML): PML is a rare but serious brain infection that can occur in patients receiving rituximab, particularly those with weakened immune systems.
- Hepatitis B Reactivation: Rituximab can reactivate hepatitis B virus (HBV) in patients who are chronic carriers of the virus.
Rituximab in Clinical Practice
Rituximab, a monoclonal antibody targeting CD20, has revolutionized the treatment of various hematological malignancies and autoimmune disorders. Its mechanism of action, targeting B cells, has led to significant improvements in patient outcomes, and its use has become increasingly widespread in clinical practice.
Rituximab in Specific Disease Subtypes
Rituximab’s therapeutic applications extend across a range of disease subtypes. It is a mainstay treatment for various B-cell malignancies, including:
- Non-Hodgkin’s lymphoma (NHL): Rituximab is commonly used in combination with chemotherapy for the treatment of various NHL subtypes, including follicular lymphoma, diffuse large B-cell lymphoma, and mantle cell lymphoma. It has demonstrated efficacy in improving response rates, prolonging remission duration, and reducing disease progression.
- Chronic lymphocytic leukemia (CLL): Rituximab is often included in treatment regimens for CLL, either as a single agent or in combination with other therapies. It has shown to be effective in reducing tumor burden and improving survival rates.
- Waldenström macroglobulinemia: Rituximab is used in combination with other agents for the treatment of Waldenström macroglobulinemia, a rare type of lymphoma characterized by the production of monoclonal immunoglobulin M (IgM). It has shown to be effective in reducing IgM levels and improving clinical symptoms.
Rituximab is also used in the management of various autoimmune disorders, including:
- Rheumatoid arthritis (RA): Rituximab is a second-line therapy for RA, used in patients who have not responded adequately to conventional disease-modifying antirheumatic drugs (DMARDs). It has shown to be effective in reducing inflammation, pain, and joint damage.
- Systemic lupus erythematosus (SLE): Rituximab is being investigated for the treatment of SLE, a chronic autoimmune disease that can affect various organs. Preliminary studies suggest that it may be effective in reducing disease activity and improving patient outcomes.
- Vasculitis: Rituximab is used in the treatment of certain types of vasculitis, such as granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA). It has shown to be effective in reducing inflammation and preventing disease progression.
Rituximab in Combination Therapies
Rituximab is often used in combination with other therapies, such as chemotherapy, other monoclonal antibodies, and targeted therapies, to enhance its efficacy and improve patient outcomes. For instance, in the treatment of NHL, rituximab is frequently combined with chemotherapy regimens, such as CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone), to improve response rates and prolong remission duration. In CLL, rituximab is often combined with other monoclonal antibodies, such as alemtuzumab or ofatumumab, to achieve synergistic effects and enhance treatment efficacy.
Impact of Rituximab on Patient Outcomes and Quality of Life
Rituximab has had a profound impact on patient outcomes and quality of life for individuals with various hematological malignancies and autoimmune disorders. It has led to significant improvements in response rates, remission duration, and overall survival in many patients. In addition, its use has been associated with improved quality of life, as it can reduce disease symptoms, such as pain, fatigue, and inflammation, enabling patients to live more active and fulfilling lives.
For example, in the treatment of NHL, rituximab has been shown to significantly improve response rates and prolong remission duration compared to chemotherapy alone. This translates to better patient outcomes and a higher quality of life. In RA, rituximab has been shown to reduce inflammation, pain, and joint damage, leading to improved function and reduced disability. This allows patients to maintain their independence and engage in activities they enjoy.
Rituximab has revolutionized the treatment of various hematological malignancies and autoimmune disorders, leading to significant improvements in patient outcomes and quality of life.
Rituximab Research and Development
Rituximab, a groundbreaking monoclonal antibody, has revolutionized the treatment of various autoimmune and hematologic malignancies. Since its initial approval in 1997, ongoing research continues to explore new applications and refine its therapeutic potential. This section delves into the dynamic landscape of rituximab research, examining ongoing investigations into novel applications, the development of biosimilars, and the future prospects of this transformative drug in the pharmaceutical arena.
New Applications for Rituximab
Research into new applications for rituximab is driven by the drug’s unique mechanism of action, targeting CD20, a protein found on the surface of B cells. This selectivity allows for targeted therapy, minimizing off-target effects. Ongoing research explores its potential in a wider range of conditions, including:
- Solid Tumors: Studies are investigating rituximab’s role in treating certain solid tumors, such as breast cancer and lung cancer, where B cells contribute to tumor growth and metastasis.
- Neurological Disorders: Researchers are exploring rituximab’s potential in treating autoimmune neurological disorders like multiple sclerosis (MS) and neuromyelitis optica spectrum disorder (NMOSD), where B cells play a role in the inflammatory process.
- Inflammatory Bowel Disease (IBD): Clinical trials are investigating rituximab’s efficacy in treating Crohn’s disease and ulcerative colitis, aiming to reduce inflammation and improve patient outcomes.
- Organ Transplantation: Rituximab’s ability to suppress B cell activity is being investigated as a potential strategy to prevent rejection in organ transplantation.
Rituximab Biosimilars
The success of rituximab has spurred the development of biosimilars, which are highly similar versions of the original drug. Biosimilars offer potential cost savings while maintaining therapeutic efficacy. The development of biosimilars is a complex process, requiring rigorous testing to demonstrate similarity to the original drug in terms of safety, efficacy, and quality.
- Regulatory Approval: Several rituximab biosimilars have received regulatory approval in various regions, expanding access to this life-saving treatment.
- Cost Considerations: Biosimilars often offer a more cost-effective alternative to the original drug, potentially improving patient access and reducing healthcare costs.
- Future of Biosimilars: The development of biosimilars is expected to continue, with ongoing research focusing on improving manufacturing processes and expanding the range of biosimilar options available.
Future Prospects of Rituximab
Rituximab’s impact on the pharmaceutical landscape is undeniable. Its success has paved the way for the development of other monoclonal antibodies, revolutionizing the treatment of various diseases. As research continues to uncover new applications and refine existing therapies, rituximab’s future prospects remain bright.
- Continued Research: Ongoing research is expected to further expand the therapeutic potential of rituximab, leading to new indications and improved treatment strategies.
- Combination Therapies: The combination of rituximab with other therapies, such as chemotherapy or targeted therapies, is a promising avenue for enhanced treatment outcomes.
- Personalized Medicine: As understanding of the role of B cells in disease pathogenesis deepens, personalized medicine approaches may emerge, tailoring rituximab treatment based on individual patient characteristics.
Rituximab: Ethical and Social Considerations
Rituximab, a monoclonal antibody, has revolutionized the treatment of various autoimmune diseases and cancers. However, its widespread use raises important ethical and social considerations that need to be carefully addressed.
Access to Treatment
Access to rituximab treatment is a crucial ethical concern. The high cost of the drug can limit its availability to patients who need it. This disparity in access can exacerbate existing health inequalities and disproportionately affect marginalized communities.
- Financial barriers: The high cost of rituximab can make it inaccessible to patients with limited financial resources, potentially leading to delayed or denied treatment.
- Insurance coverage: Coverage for rituximab can vary significantly depending on insurance plans, creating a barrier for patients with less comprehensive insurance.
- Geographic disparities: Access to rituximab can be limited in rural areas or underserved communities due to limited availability of specialists and healthcare facilities.
Social Impact on Patients and Families
The use of rituximab can have a significant impact on patients and their families.
- Treatment-related side effects: Rituximab can cause side effects, including infections, infusion reactions, and long-term complications. This can impact the quality of life of patients and require significant support from families.
- Emotional and psychological burden: The diagnosis and treatment of serious conditions can be emotionally challenging for patients and their families. The potential for long-term treatment with rituximab can add to this burden.
- Impact on daily life: The treatment regimen for rituximab can involve frequent hospital visits and time off work, potentially impacting the daily lives of patients and their families.
Patient Education and Informed Consent
Patient education and informed consent are crucial for ensuring ethical and responsible use of rituximab.
- Understanding the risks and benefits: Patients need to be fully informed about the potential benefits and risks of rituximab treatment, including its effectiveness, side effects, and long-term implications.
- Shared decision-making: Patients should be actively involved in the decision-making process regarding their treatment, considering their values and preferences.
- Ongoing communication: Open and honest communication between healthcare providers and patients is essential throughout the treatment process, ensuring that patients are fully informed and supported.
Rituximab: A Case Study Approach

Rituximab, a monoclonal antibody, is widely used in the treatment of various autoimmune diseases and cancers. Understanding its application in a real-world scenario can provide valuable insights into its clinical efficacy and challenges. This case study explores the use of rituximab in a patient with rheumatoid arthritis.
Case Study: Rheumatoid Arthritis
This case study involves a 55-year-old female patient diagnosed with rheumatoid arthritis (RA). She presented with persistent joint pain, stiffness, and swelling, primarily affecting her hands and feet. Despite initial treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) and disease-modifying antirheumatic drugs (DMARDs), her symptoms remained uncontrolled.
The patient’s treatment plan included rituximab, a B-cell depleting agent, in combination with methotrexate, a DMARD. The rationale for using rituximab was based on its ability to target and deplete B-cells, which are known to play a significant role in the pathogenesis of RA.
Following the initiation of rituximab therapy, the patient experienced a significant improvement in her symptoms. Her joint pain, stiffness, and swelling decreased considerably, leading to improved mobility and quality of life.
Challenges and Considerations
The management of this patient’s case presented several challenges and considerations:
- Monitoring for Adverse Effects: Rituximab can cause various adverse effects, including infusion reactions, infections, and hematological abnormalities. Close monitoring of the patient’s condition is crucial to identify and manage any potential complications.
- Infusion Reactions: The patient experienced mild infusion reactions, including fever and chills, during the initial rituximab infusions. Premedication with antihistamines and corticosteroids helped to mitigate these reactions.
- Risk of Infections: Rituximab’s B-cell depleting action can increase the risk of infections. The patient’s immune status was closely monitored, and prophylactic antibiotics were prescribed to prevent infections.
- Long-Term Efficacy: Rituximab’s efficacy can vary between patients, and some individuals may experience a loss of response over time. Continued monitoring and adjustments to the treatment plan may be necessary to maintain symptom control.
Despite these challenges, the patient’s response to rituximab therapy was positive, and she continues to benefit from its effects. This case study illustrates the potential benefits of rituximab in treating rheumatoid arthritis, highlighting its efficacy in achieving symptom control and improving quality of life. However, it also emphasizes the importance of careful patient selection, close monitoring for adverse effects, and ongoing management to ensure optimal outcomes.
Rituximab: Future Directions

Rituximab has revolutionized the treatment of various cancers and autoimmune diseases. Its success has paved the way for further research and development, aiming to enhance its efficacy and expand its therapeutic applications. This section explores the promising avenues for future directions of rituximab.
Repurposing Rituximab for New Therapeutic Applications
The potential for repurposing rituximab for new therapeutic applications is significant.
- Treating other B-cell malignancies: While primarily used for non-Hodgkin lymphoma, rituximab’s efficacy in targeting B-cells makes it a potential candidate for treating other B-cell malignancies, such as chronic lymphocytic leukemia (CLL) and Waldenstrom macroglobulinemia.
- Treating autoimmune diseases: Rituximab’s success in rheumatoid arthritis has spurred research into its potential for treating other autoimmune diseases, including systemic lupus erythematosus (SLE) and inflammatory bowel disease (IBD). Clinical trials are underway to evaluate its efficacy in these conditions.
- Treating solid tumors: Recent studies suggest that rituximab may have activity against certain solid tumors, such as breast cancer and lung cancer. Further research is needed to determine its efficacy and optimal use in these settings.
Rituximab’s impact on healthcare is undeniable. It has significantly improved patient outcomes, offering a targeted approach to treating complex diseases. The development of biosimilars has also expanded access to this life-changing therapy. Ongoing research continues to explore new applications and enhance the efficacy and safety of rituximab, promising even greater benefits for patients in the future.
Rituximab is a powerful medication used to treat certain types of cancer and autoimmune disorders. While it works by targeting specific immune cells, it doesn’t address addiction issues, which are often treated with medications like vivitrol. Vivitrol, a long-acting injectable medication, helps prevent relapse in individuals struggling with opioid addiction. Rituximab, on the other hand, focuses on immune system regulation, highlighting the diverse approaches employed in modern medicine to address various health challenges.