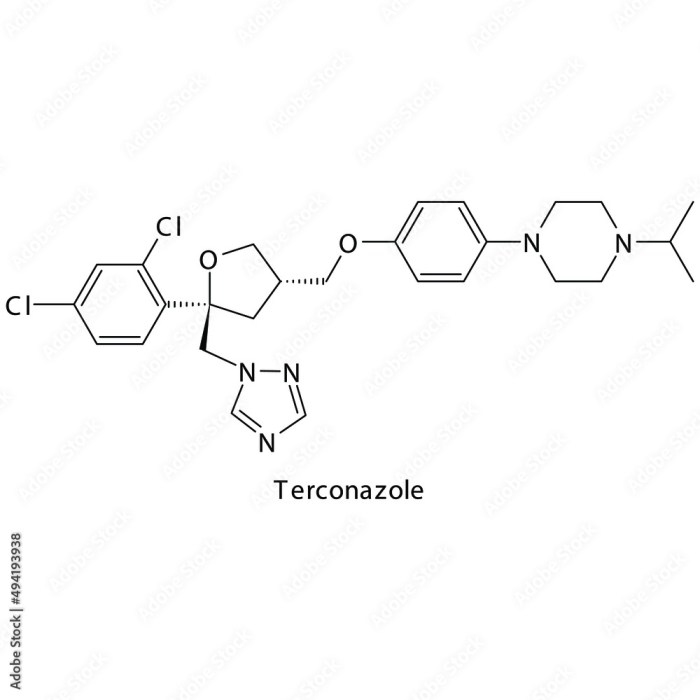
Terconazole, a potent antifungal medication, stands as a powerful weapon against a wide range of fungal infections, particularly vaginal yeast infections (candidiasis). Its effectiveness stems from its ability to disrupt the growth and reproduction of fungi, effectively combating these troublesome infections.
This comprehensive overview delves into the intricacies of terconazole, exploring its chemical structure, mechanism of action, therapeutic applications, pharmacokinetics, safety profile, dosage recommendations, and comparison to other antifungal agents. We’ll also delve into the latest research and development efforts surrounding terconazole and its potential future applications.
Therapeutic Applications: Terconazole

Terconazole is an antifungal medication that belongs to the imidazole class of drugs. It works by inhibiting the growth of certain types of fungi, including Candida species, which are responsible for many common fungal infections.
Terconazole is primarily used to treat vaginal yeast infections, also known as candidiasis. It is available in various forms, including vaginal cream, suppositories, and tablets.
Treatment of Vaginal Yeast Infections
Vaginal yeast infections are a common condition that affects many women. These infections occur when there is an overgrowth of Candida fungi in the vagina. Terconazole is effective in treating vaginal yeast infections because it directly targets and kills the Candida fungi, restoring the balance of microorganisms in the vagina.
Several clinical studies have demonstrated the effectiveness of terconazole in treating vaginal yeast infections. In a randomized, double-blind, placebo-controlled trial involving women with vulvovaginal candidiasis, terconazole cream was found to be significantly more effective than placebo in relieving symptoms and achieving clinical cure.
Treatment of Other Fungal Infections, Terconazole
Terconazole is also used to treat other fungal infections, such as:
- Skin infections: Terconazole can be used to treat fungal infections of the skin, such as athlete’s foot, jock itch, and ringworm.
- Oral thrush: Terconazole can be used to treat oral thrush, a fungal infection of the mouth that is common in infants and immunocompromised individuals.
Pharmacokinetics and Metabolism
Terconazole’s pharmacokinetic profile describes its absorption, distribution, metabolism, and elimination within the body. Understanding these processes is crucial for determining optimal dosing regimens and predicting potential drug interactions.
Absorption
Terconazole is a topical antifungal agent, meaning it is applied directly to the skin or mucous membranes. Upon application, it is absorbed systemically to a limited extent.
- The extent of absorption can vary depending on the specific formulation, site of application, and the integrity of the skin or mucous membrane.
- Absorption is generally low, with only a small amount of the drug reaching the bloodstream.
Distribution
After absorption, terconazole is distributed throughout the body. It is primarily distributed to the skin and mucous membranes, where it exerts its antifungal effects.
- It has a relatively low volume of distribution, suggesting that it is mainly confined to the bloodstream and tissues.
- Terconazole is not known to accumulate significantly in any particular organ or tissue.
Metabolism
Terconazole is metabolized in the liver, primarily through cytochrome P450 enzymes. This metabolic process transforms the drug into inactive metabolites.
- The specific metabolic pathways involved in terconazole metabolism have not been fully characterized.
- It is important to note that terconazole metabolism can be influenced by factors such as age, liver function, and the presence of other medications.
Elimination
Terconazole is eliminated from the body primarily through the feces, with a smaller amount excreted in the urine.
- The elimination half-life of terconazole is approximately 12 hours, indicating that it is eliminated from the body relatively quickly.
- The rate of elimination can be affected by factors such as renal function and the presence of other medications.
Factors Influencing Pharmacokinetics
Several factors can influence the pharmacokinetic profile of terconazole, including:
- Age: Elderly patients may have reduced liver and kidney function, which could affect the metabolism and elimination of terconazole.
- Liver function: Patients with impaired liver function may experience slower metabolism and increased drug accumulation.
- Renal function: Patients with impaired renal function may experience slower elimination of terconazole, leading to increased drug levels in the body.
- Pregnancy and lactation: Terconazole is not recommended for use during pregnancy or lactation due to potential risks to the fetus or infant.
- Concomitant medications: Certain medications can interact with terconazole, affecting its absorption, metabolism, or elimination.
Drug Interactions
The potential for drug interactions with terconazole is relatively low due to its limited systemic absorption. However, it is important to be aware of potential interactions with medications that are metabolized by the same cytochrome P450 enzymes.
- CYP3A4 inhibitors: Medications that inhibit CYP3A4, such as ketoconazole, itraconazole, and erythromycin, could potentially increase terconazole levels in the body by slowing down its metabolism.
- CYP3A4 inducers: Medications that induce CYP3A4, such as rifampin and phenytoin, could potentially decrease terconazole levels in the body by speeding up its metabolism.
Terconazole emerges as a valuable therapeutic option for treating fungal infections, particularly vaginal yeast infections. Its effectiveness, safety profile, and ease of administration make it a reliable choice for patients seeking relief from these conditions. However, it’s crucial to consult a healthcare professional for personalized advice and to ensure the safe and effective use of terconazole.
Terconazole is a common antifungal medication used to treat vaginal yeast infections. While it effectively combats fungal growth, it’s important to remember that terconazole doesn’t address the underlying hormonal imbalances that can contribute to recurring infections. For these situations, medications like mifepristone , which work on a different level, may be considered. Ultimately, the best approach for treating yeast infections involves a thorough understanding of the individual’s health history and a personalized treatment plan.