Unasyn, a powerful antibiotic, has been a cornerstone of medical treatment for decades. Its unique chemical composition and broad spectrum of activity have made it a valuable tool in combating bacterial infections. This article delves into the intricate world of Unasyn, exploring its mechanism of action, medical applications, potential interactions and side effects, and its role in the fight against antimicrobial resistance.
Unasyn, a combination of ampicillin and sulbactam, is a semi-synthetic penicillin antibiotic. Its effectiveness lies in its ability to inhibit bacterial cell wall synthesis, ultimately leading to bacterial cell death. Unasyn is particularly effective against a wide range of gram-positive and gram-negative bacteria, including those that have developed resistance to other antibiotics.
Understanding Unasyn
Unasyn, also known as sulbactam/ampicillin, is a powerful antibiotic used to treat a wide range of bacterial infections. It is a combination drug consisting of two components: ampicillin, a penicillin-like antibiotic, and sulbactam, a beta-lactamase inhibitor.
Chemical Composition
Unasyn is a combination of ampicillin and sulbactam. Ampicillin is a semisynthetic penicillin antibiotic that inhibits bacterial cell wall synthesis by interfering with the formation of peptidoglycan, a crucial component of the bacterial cell wall. Sulbactam is a beta-lactamase inhibitor, which means it prevents the breakdown of ampicillin by bacterial enzymes called beta-lactamases. Beta-lactamases are produced by certain bacteria to inactivate penicillin antibiotics, rendering them ineffective.
Mechanism of Action
Unasyn’s mechanism of action is based on the synergistic effect of its two components. Ampicillin acts as the primary antibacterial agent, targeting the synthesis of bacterial cell walls. Sulbactam, on the other hand, protects ampicillin from enzymatic degradation by beta-lactamases, ensuring that ampicillin can effectively reach its target and exert its antibacterial effect.
Types of Bacteria Unasyn is Effective Against
Unasyn is effective against a wide range of bacteria, including both gram-positive and gram-negative organisms. Some examples of bacteria susceptible to Unasyn include:
- Streptococcus pneumoniae
- Staphylococcus aureus (including methicillin-sensitive strains)
- Haemophilus influenzae
- Escherichia coli
- Proteus mirabilis
- Klebsiella pneumoniae
Medical Applications of Unasyn
Unasyn, a combination antibiotic, is commonly used to treat a variety of bacterial infections. It is effective against a wide range of bacteria, making it a versatile treatment option for several medical conditions.
Common Medical Conditions Treated with Unasyn
Unasyn is primarily used to treat serious bacterial infections, particularly those affecting the respiratory, skin, and urinary tracts. It is also effective in treating infections in the abdomen and pelvis. Here are some of the common medical conditions that Unasyn is used to treat:
- Pneumonia: Unasyn is effective against various bacteria that cause pneumonia, including *Streptococcus pneumoniae*, *Haemophilus influenzae*, and *Moraxella catarrhalis*.
- Skin Infections: Unasyn can be used to treat skin infections such as cellulitis, abscesses, and wound infections caused by susceptible bacteria.
- Urinary Tract Infections (UTIs): Unasyn is effective against many bacteria that cause UTIs, including *Escherichia coli*, *Proteus mirabilis*, and *Klebsiella pneumoniae*.
- Abdominal Infections: Unasyn can be used to treat infections in the abdomen, such as peritonitis and intra-abdominal abscesses.
- Pelvic Inflammatory Disease (PID): Unasyn is often used to treat PID, a serious infection of the reproductive organs in women.
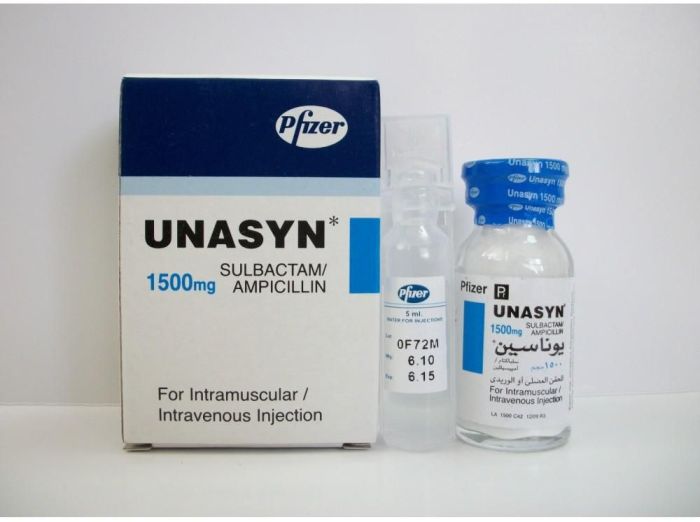
Dosage Forms and Uses
Unasyn is available in two dosage forms:
- Intravenous (IV) Injection: This form is typically used for serious infections requiring immediate treatment, such as pneumonia or sepsis. It allows for rapid absorption and delivery of the medication directly into the bloodstream.
- Intramuscular (IM) Injection: This form is used for infections that are not as severe or when IV access is not readily available. It provides a slower release of the medication into the bloodstream.
Dosage Regimen and Duration of Treatment
The dosage regimen and duration of Unasyn treatment depend on the severity of the infection, the patient’s age, and overall health.
The recommended dosage for adults is typically 1.5 to 3 grams of Unasyn every 6 to 8 hours.
Treatment duration usually ranges from 7 to 14 days, but it can vary depending on the individual case. It is crucial to complete the entire course of treatment, even if symptoms improve, to ensure the infection is completely eradicated.
Unasyn in Different Patient Populations
Unasyn’s use in various patient populations, particularly those with unique physiological considerations, requires careful evaluation and potential adjustments to ensure safety and efficacy. This section explores the considerations for using Unasyn in pregnant women, breastfeeding mothers, children, and elderly patients.
Unasyn in Pregnant Women
Unasyn is classified as a pregnancy category B drug, indicating that studies in animals have not shown harm to the fetus, but there are no adequate and well-controlled studies in pregnant women. While Unasyn is generally considered safe for use during pregnancy, it’s crucial to weigh the potential benefits against the potential risks.
- Potential Risks: While Unasyn is generally considered safe during pregnancy, it’s important to note that all medications can potentially pose risks to the developing fetus. For example, Unasyn may cross the placenta and could potentially affect the fetus’s development. However, these risks are generally considered low.
- Benefits: In situations where the benefits of treating the infection outweigh the potential risks, Unasyn may be prescribed during pregnancy. For example, Unasyn might be used to treat serious infections that could threaten the mother’s health and, consequently, the fetus.
- Monitoring: Regular monitoring of the mother and fetus is essential during Unasyn treatment. This may include monitoring the mother’s blood pressure, fetal heart rate, and fetal growth.
Unasyn in Breastfeeding Mothers
Unasyn is excreted in breast milk, and it’s important to consider the potential risks to the infant.
- Potential Risks: Unasyn may be passed to the infant through breast milk, potentially causing adverse effects. These effects could include diarrhea, diaper rash, or yeast infections.
- Benefits: In some cases, the benefits of treating the mother’s infection with Unasyn may outweigh the potential risks to the infant. This decision is best made in consultation with a healthcare professional.
- Alternatives: If possible, alternative medications that are considered safer for breastfeeding mothers may be considered.
Unasyn in Children
The use of Unasyn in children requires careful consideration and potential adjustments to dosage.
- Dosage: The dosage of Unasyn for children is typically based on their weight and age.
- Safety: Unasyn is generally safe and effective in children, but it’s essential to monitor for any adverse effects.
- Monitoring: Close monitoring of the child’s response to Unasyn is crucial. This may include monitoring for signs of infection, such as fever, and for any potential side effects.
Unasyn in Elderly Patients
Elderly patients may have a higher risk of developing adverse effects from Unasyn.
- Increased Risk: Elderly patients may have reduced kidney and liver function, which can affect how Unasyn is metabolized and eliminated from the body.
- Dosage Adjustments: Dosage adjustments may be necessary in elderly patients to reduce the risk of side effects.
- Monitoring: Close monitoring for adverse effects is crucial in elderly patients.
Unasyn and its Alternatives

Unasyn, a combination antibiotic, is often prescribed for a variety of infections. However, it’s important to understand that Unasyn isn’t the only option available. Several other antibiotics can effectively treat similar conditions, each with its own set of advantages and disadvantages. This section will delve into these alternatives, comparing and contrasting them with Unasyn to help you make informed decisions about your treatment.
Comparison of Unasyn and its Alternatives
Understanding the differences between Unasyn and its alternatives requires examining their mechanisms of action, effectiveness against specific infections, and potential side effects. This information is crucial for healthcare providers to select the most appropriate antibiotic for each patient, considering factors like the type of infection, the patient’s medical history, and potential drug interactions.
- Unasyn (ampicillin/sulbactam): A combination antibiotic containing ampicillin, a penicillin-type antibiotic, and sulbactam, a beta-lactamase inhibitor. Unasyn works by inhibiting bacterial cell wall synthesis, preventing bacteria from multiplying. It’s effective against a wide range of gram-positive and gram-negative bacteria, including some that are resistant to ampicillin alone. However, Unasyn can cause allergic reactions, gastrointestinal disturbances, and may interact with other medications.
- Augmentin (amoxicillin/clavulanate): Another combination antibiotic containing amoxicillin, a penicillin-type antibiotic, and clavulanate, a beta-lactamase inhibitor. Augmentin’s mechanism of action is similar to Unasyn, inhibiting bacterial cell wall synthesis. It’s also effective against a broad spectrum of bacteria, including those resistant to amoxicillin alone. Like Unasyn, Augmentin can cause allergic reactions, gastrointestinal disturbances, and may interact with other medications.
- Zosyn (piperacillin/tazobactam): A combination antibiotic containing piperacillin, a penicillin-type antibiotic, and tazobactam, a beta-lactamase inhibitor. Zosyn’s mechanism of action is similar to Unasyn and Augmentin, inhibiting bacterial cell wall synthesis. It’s particularly effective against Pseudomonas aeruginosa, a common cause of hospital-acquired infections. Zosyn can cause allergic reactions, gastrointestinal disturbances, and may interact with other medications.
- Cefazolin: A cephalosporin antibiotic that works by inhibiting bacterial cell wall synthesis. It’s effective against a wide range of gram-positive and some gram-negative bacteria. Cefazolin is typically administered intravenously and is often used to treat skin infections, respiratory infections, and surgical prophylaxis. It can cause allergic reactions, gastrointestinal disturbances, and may interact with other medications.
- Vancomycin: A glycopeptide antibiotic that works by inhibiting bacterial cell wall synthesis. It’s effective against gram-positive bacteria, including those resistant to penicillin and cephalosporin antibiotics. Vancomycin is typically administered intravenously and is often used to treat serious infections, such as MRSA (methicillin-resistant Staphylococcus aureus). It can cause allergic reactions, kidney problems, and may interact with other medications.
Advantages and Disadvantages of Unasyn
Unasyn offers several advantages over other antibiotics, including its broad-spectrum activity, effectiveness against penicillin-resistant bacteria, and availability in both intravenous and oral forms. However, it also has some drawbacks, such as potential allergic reactions, gastrointestinal disturbances, and interactions with other medications.
Advantages of Unasyn
- Broad-spectrum activity: Unasyn is effective against a wide range of bacteria, making it suitable for treating various infections.
- Effectiveness against penicillin-resistant bacteria: The sulbactam component of Unasyn inhibits beta-lactamases, enzymes produced by bacteria that can inactivate penicillin-type antibiotics. This makes Unasyn effective against bacteria that are resistant to ampicillin alone.
- Availability in both intravenous and oral forms: Unasyn is available for both intravenous and oral administration, providing flexibility in treatment options.
Disadvantages of Unasyn
- Allergic reactions: Like other penicillin-type antibiotics, Unasyn can cause allergic reactions, including anaphylaxis.
- Gastrointestinal disturbances: Unasyn can cause gastrointestinal disturbances, such as diarrhea, nausea, and vomiting.
- Drug interactions: Unasyn can interact with other medications, potentially affecting their effectiveness or increasing the risk of side effects.
Antibiotic Suitability for Specific Infections
The choice of antibiotic for a specific infection depends on various factors, including the type of bacteria causing the infection, the patient’s medical history, and potential drug interactions. The table below provides a general overview of the suitability of different antibiotics for common infections.
| Antibiotic | Mechanism of Action | Suitable Infections |
|---|---|---|
| Unasyn (ampicillin/sulbactam) | Inhibits bacterial cell wall synthesis | Skin infections, respiratory infections, urinary tract infections, ear infections, and some types of pneumonia |
| Augmentin (amoxicillin/clavulanate) | Inhibits bacterial cell wall synthesis | Similar to Unasyn, but may be preferred for certain infections, such as otitis media (ear infections) |
| Zosyn (piperacillin/tazobactam) | Inhibits bacterial cell wall synthesis | Severe infections, including those caused by Pseudomonas aeruginosa, hospital-acquired pneumonia, and complicated skin infections |
| Cefazolin | Inhibits bacterial cell wall synthesis | Skin infections, respiratory infections, surgical prophylaxis |
| Vancomycin | Inhibits bacterial cell wall synthesis | Serious infections, including those caused by MRSA (methicillin-resistant Staphylococcus aureus) |
Unasyn’s Role in Antimicrobial Resistance
Unasyn, like all antibiotics, carries the potential to contribute to the development of antibiotic resistance. This is a critical concern in healthcare, as the emergence of resistant bacteria threatens the effectiveness of our current arsenal of antimicrobial drugs. Understanding the factors that contribute to resistance and implementing strategies to mitigate its development is essential for maintaining the efficacy of Unasyn and other antibiotics.
Strategies to Mitigate the Risk of Antibiotic Resistance Related to Unasyn Use
The judicious use of antibiotics is crucial to minimize the risk of resistance. This involves a multi-pronged approach that focuses on optimizing treatment strategies and promoting responsible antibiotic use.
- Prescribing Unasyn Only When Necessary: Unasyn should only be prescribed for infections confirmed to be caused by susceptible bacteria. This minimizes unnecessary exposure to the antibiotic, reducing the selective pressure that can drive resistance development.
- Prescribing the Correct Dose and Duration: Adequate doses of Unasyn should be administered for the full duration of treatment. This ensures the eradication of the infecting bacteria and minimizes the risk of incomplete eradication, which can lead to the selection of resistant strains.
- Promoting Infection Prevention and Control Measures: Strict adherence to infection control practices, such as hand hygiene and appropriate isolation techniques, can significantly reduce the spread of resistant bacteria. This helps prevent the emergence and dissemination of resistant strains within healthcare settings.
- Developing and Implementing Antimicrobial Stewardship Programs: Antimicrobial stewardship programs play a critical role in promoting the responsible use of antibiotics. These programs involve pharmacists, physicians, and other healthcare professionals who work collaboratively to optimize antibiotic use, monitor resistance patterns, and educate healthcare providers and patients about antibiotic resistance.
Unasyn’s Impact on the Human Microbiome
Unasyn, like many antibiotics, can disrupt the delicate balance of the human microbiome, the diverse community of microorganisms residing in our gut and other parts of the body. Understanding the potential impact of Unasyn on the microbiome is crucial for optimizing its use and mitigating any adverse effects.
Potential Impact on Microbiome Composition and Function
Unasyn’s broad-spectrum activity targets not only pathogenic bacteria but also beneficial commensal bacteria residing in the gut. This can lead to alterations in the composition and function of the microbiome. The reduction in beneficial bacteria, such as those involved in nutrient metabolism and immune system development, can have far-reaching consequences for overall health.
Potential Consequences of Altering the Microbiome
The disruption of the microbiome due to Unasyn use can contribute to various health issues. These include:
- Increased susceptibility to infections: The loss of beneficial bacteria can weaken the gut’s natural defense mechanisms, making individuals more vulnerable to infections by opportunistic pathogens.
- Digestive problems: Unasyn-induced dysbiosis can lead to digestive issues like diarrhea, constipation, and abdominal pain.
- Immune system dysregulation: The microbiome plays a vital role in immune system development and regulation. Alterations in the microbiome can lead to immune dysregulation, increasing the risk of autoimmune disorders and allergies.
- Metabolic disorders: The microbiome is involved in metabolism and energy regulation. Disruption of the microbiome can contribute to metabolic disorders like obesity and type 2 diabetes.
Strategies to Mitigate Microbiome Impact
While Unasyn’s impact on the microbiome can be significant, strategies exist to mitigate these effects:
- Probiotic supplementation: Probiotics, containing live beneficial bacteria, can help restore the balance of the microbiome after antibiotic use. They can replenish the gut with beneficial bacteria, aiding in digestion, immune function, and overall health.
- Prebiotic intake: Prebiotics are non-digestible fibers that serve as food for beneficial bacteria in the gut. They promote the growth and activity of these beneficial bacteria, contributing to a healthier microbiome.
- Fecal microbiota transplantation (FMT): In severe cases of antibiotic-associated dysbiosis, FMT may be considered. This involves transferring healthy gut bacteria from a donor to the recipient’s gut, aiming to restore a healthy microbiome.
Research and Development Related to Unasyn
Unasyn, a combination antibiotic, has been a mainstay in treating various infections for decades. However, ongoing research and development efforts continue to explore new applications, formulations, and strategies to enhance its efficacy and address emerging challenges.
Ongoing Research Studies
Ongoing research studies related to Unasyn are exploring its clinical applications in various settings, including:
- Treating complicated skin and skin structure infections (cSSSI): Studies are investigating the efficacy and safety of Unasyn in treating cSSSI, particularly in patients with comorbidities, such as diabetes or immunosuppression.
- Treating infections in immunocompromised patients: Research is examining the role of Unasyn in managing infections in patients with weakened immune systems, such as those undergoing chemotherapy or organ transplantation.
- Evaluating Unasyn’s effectiveness against emerging antibiotic-resistant bacteria: Studies are exploring the potential of Unasyn in treating infections caused by multidrug-resistant organisms, particularly in hospital settings.
Potential for New Formulations and Delivery Methods
The development of novel formulations and delivery methods for Unasyn is an active area of research. These advancements aim to:
- Improve drug bioavailability: Researchers are exploring new formulations that enhance the absorption and distribution of Unasyn in the body, potentially leading to improved efficacy.
- Target drug delivery: Targeted drug delivery systems are being investigated to deliver Unasyn directly to the site of infection, potentially reducing systemic side effects and improving therapeutic outcomes.
- Develop extended-release formulations: Extended-release formulations could provide sustained drug levels over a longer period, potentially simplifying dosing regimens and improving patient compliance.
Potential for New Antibiotic Therapies
The emergence of antibiotic resistance poses a significant challenge to global health. Researchers are actively exploring new antibiotic therapies to address this threat. Some promising avenues include:
- Developing new antibiotic classes: Research is focused on identifying and developing novel antibiotics that target different bacterial pathways, potentially circumventing existing resistance mechanisms.
- Modifying existing antibiotics: Researchers are exploring ways to modify existing antibiotics, such as Unasyn, to overcome resistance mechanisms and enhance their effectiveness.
- Combinatorial therapies: Combining existing antibiotics with novel agents or other therapeutic strategies, such as phage therapy or immunotherapy, may offer a synergistic approach to combating antibiotic resistance.
Unasyn has undoubtedly played a vital role in combating bacterial infections, but the rise of antimicrobial resistance necessitates careful consideration of its use. Understanding its mechanisms, potential side effects, and interactions is crucial for responsible and effective treatment. As research continues to unravel the complexities of Unasyn and its impact on the human microbiome, we can expect to see further advancements in its application and the development of alternative therapies.
Unasyn is a powerful antibiotic often used to treat serious bacterial infections. While it’s effective, it’s important to remember that not all infections respond to the same treatments. For example, certain types of diabetes might require insulin, like Humulin N , which is a long-acting insulin designed to provide steady blood sugar control throughout the day. Understanding the different types of treatments available is crucial for effective healthcare management.